Your Rights and Protections Against Surprise Medical Bills

Your Rights and Protections Against Surprise Medical Bills
When you get emergency care or are treated by an out-of-network provider at an in-network hospital or ambulatory surgical center, you are protected from balance billing. In these cases, you shouldn’t be charged more than your plan’s copayments, coinsurance and/or deductible.
WHAT IS “BALANCE BILLING” (SOMETIMES CALLED “SURPRISE BILLING”)?
When you see a doctor or other health care provider, you may owe certain out-of-pocket costs, like a copayment, coinsurance, or deductible. You may have additional costs or have to pay the entire bill if you see a provider or visit a health care facility that isn’t in your health plan’s network.
“Out-of-network” means providers and facilities that haven’t signed a contract with your health plan to provide services. Out-of-network providers may be allowed to bill you for the difference between what your plan pays and the full amount charged for a service. This is called “balance billing.” This amount is likely more than in-network costs for the same service and might not count toward your plan’s deductible or annual out-of-pocket limit.
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in- network facility but are unexpectedly treated by an out-of-network provider. Surprise medical bills could cost thousands of dollars depending on the procedure or service.
YOU’RE PROTECTED FROM BALANCE BILLING FOR:
Emergency services
If you have an emergency medical condition and get emergency services from an out-of- network provider or facility, the most they can bill you is your plan’s in-network cost- sharing amount (such as copayments, coinsurance, and deductibles). You can’t be balance billed for these emergency services. This includes services you may get after you’re in stable condition, unless you give written consent and give up your protections not to be balanced billed for these post-stabilization services.
Connecticut passed its own law in 2015 to address balance billing. The law applies to health plans regulated by Connecticut’s Department of Insurance and has similar protections to those provided under the federal No Surprises Act. For more information, see: For more information, see Stat. §§ 38a-477aa and 20-7f or the Connecticut Department of Insurance website at
portal.ct.gov/CID/General-Consumer-Information/No-Surprises-Act.
Certain services at an in-network hospital or ambulatory surgical center
When you get services from an in-network hospital or ambulatory surgical center, certain providers there may be out-of-network. In these cases, the most those providers can bill you is your plan’s in-network cost-sharing amount. This applies to emergency medicine, anesthesia, pathology, radiology, laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can not balance bill you and may not ask you to give up your protections not to be balance billed.
If you get other types of services at these in-network facilities, out-of-network providers can’t balance bill you, unless you give written consent and give up your protections.
You are never required to give up your protections from balance billing. You also aren’t required to get out-of-network care. You can choose a provider or facility in your plan’s network.
Connecticut passed its own law in 2015 to address balance billing. The law applies to health plans regulated by Connecticut’s Department of Insurance and has similar protections to those provided under the federal No Surprises Act. For more information, see
portal.ct.gov/CID/General-Consumer-Information/No-Surprises-Act.
When balance billing isn’t allowed, you also have these protections:
o Cover emergency services without requiring you to get approval for services in advance (also known as “prior authorization”).
- You’re only responsible for paying your share of the cost (like the copayments, coinsurance, and deductible that you would pay if the provider or facility was in- network). Your health plan will pay any additional costs to out-of-network providers and facilities directly.
- Generally, your health plan must:
o Cover emergency services by out-of-network providers.
o Base what you owe the provider or facility (cost-sharing) on what it would pay an in-network provider or facility and show that amount in your explanation of benefits.
o Count any amount you pay for emergency services or out-of-network services toward your in-network deductible and out-of-pocket limit.
If you think you’ve been wrongly billed, contact:
- Connecticut Department of Insurance: portal.ct.gov/CID/Consumer-Affairs/File-a- Complaint-or-Ask-a-Question or Consumer Helpline: 800-203-3447 or 860-297-3900
- The State of Connecticut Office of the Healthcare Advocate at 866-466-4446 or Healthcare.advocate@ct.gov.
- If you think you’ve been wrongly billed and your coverage is subject to New York law you may contact the New York State Department of Financial services at 1-800-342-3736 or surprisemedicalbills@dfs.ny.gov. Visit www.dfs.ny.gov for information about your rights under state law.
- Visit cms.gov/nosurprises/consumers for more information about your rights under federal law.
About Dr. Erhard

About Dr. Erhard
Breast Reconstruction Specialist - New York and Connecticut
Heather Erhard, MD, FACS is a Board Certified Plastic Surgeon who specializes in reconstruction and aesthetic surgery of the breast. Surgery of the breast represents the vast majority of her practice, however, Dr. Erhard also has significant experience with surgery of the trunk and body, including post-bariatric body contouring.
After completing a surgical residency in General Surgery, Dr. Erhard achieved board certification in General Surgery and became a Fellow of the American College of Surgeons. She completed a Plastic and Reconstructive surgery residency at Montefiore Medical Center under the supervision of pioneering microsurgeon, Dr. Berish Strauch. After completing training at Montefiore and the Albert Einstein College of Medicine, Dr. Erhard completed two additional subspecialty fellowships, training in microvascular perforator flap breast reconstruction with Dr. Robert Allen at Louisiana State University and in cosmetic and aesthetic surgery with Dr. Donald Wood-Smith in Manhattan. Combined subspecialty training in both aesthetic surgery and microvascular surgery has helped Dr. Erhard to truly refine the cosmetic results of the reconstructive procedures that she performs.
Dr. Erhard introduced perforator flap breast reconstruction to Montefiore Medical Center in 2004. Together with a team of dedicated individuals, she performed the first Deep Inferior Epigastric Perforator (DIEP) flap at Montefiore Medical Center, followed by the first Gluteal Artery Perforator (GAP), Transverse Upper Gracilis (TUG), conjoined (stacked) DIEP, Thoracodorsal Artery Perforator (TDAP), and Lumbar Artery Perforator (LAP) flaps to be done there. She assisted in the introduction of perforator flap reconstruction at both Greenwich Hospital in Greenwich, Connecticut and Vassar Brothers Medical Center in Poughkeepsie, New York. She now provides services to meet the reconstructive needs of patients in the Bronx, the Hudson Valley, and Connecticut, with privileges at multiple institutions.
In addition to being a Fellow of the American College of Surgeons, Dr. Erhard is a member of many surgical societies including the American Society of Plastic Surgeons, the American Society for Reconstructive Microsurgery, and the World Society for Reconstructive Microsurgery. She is an Assistant Clinical Professor of Surgery at the Albert Einstein College of Medicine-Montefiore Medical Center, where she instructs surgical residents and physician assistants in-training, participates in Quality Assurance reviews, and assesses residents during mock oral board examinations. Dr. Erhard also helps train medical students and residents at Montefiore Medical Center and Vassar Brothers Medical Center.
Dr. Erhard trained together with Dr. David Greenspun at Montefiore Medical Center and the Albert Einstein College of Medicine. Following training, in 2004, they began working together, and in over 15 years have performed more than 1,500 breast reconstructions. Their partnership is one of mutual respect with dedication to the highest level of personalized patient care.
Dr. Erhard lives in New York City with her husband, daughter, and labradoodle. Outside of work she enjoys spending time traveling, reading, and visiting with her large extended family.
» Contact us if you would like to make an appointment and learn more about your options
Implant vs Natural Tissue Reconstruction

All breast reconstruction procedures fall into one of two broad categories:
- Breast reconstruction using natural tissue from your own body
- Breast reconstruction using breast implants
The surgeons of the Advanced Reconstructive Surgery Group specialize breast reconstruction surgery.
Some of the key differences between natural-tissue breast reconstruction using perforator flaps such as the DIEP flap and implant breast reconstruction are summarized in the table below.
| IMPLANTS | FLAPS | |
|---|---|---|
| Material Used | Uses silicone or saline-filled implant | Uses a person’s own natural tissue |
| Long-term results | Implants generally don’t last forever—most women have an implant replaced one or more times during their lifetime | Flaps are permanent and never need to be replaced |
| Failure rate | FDA data shows that about 30% of implants are removed within 10 years | Our practice performs DIEP flaps with a success rate of at least 99.5% |
| Breast consistency | Breasts reconstructed with implants typically feel firmer and cooler to the touch than normal body temperature | Breasts reconstructed with natural tissue are soft and warm much like a natural breast |
| Breast sensation | Minimal to no return of sensation | To a variable degree, sensation frequently returns |
| Surgery time | Mastectomy with implant reconstruction typically takes about 2-3 hours | Mastectomy with DIEP flap reconstruction typically takes 3.5-5.5 hours |
| Hospital stay | Typical hospital stay is 1 night | Typical hospital stay is 2-3 nights |
| Number of procedures | Two procedures are usually needed to complete the reconstruction, though sometimes it can be done in with just a single procedure | Two procedures are usually needed to complete breast reconstruction using a woman’s own natural tissue |
| Recovery highlights | Most women can drive within 2 weeks of surgery and resume light exercise at 4-6 weeks | Most women can drive within 2-3 weeks of surgery and resume light exercise at 4-6 weeks |
Material Used
Implants
Uses silicone or saline-filled implant
Flaps
Uses a person’s own natural tissue
Long-term results
Implants
Implants generally don’t last forever—most women have an implant replaced one or more times during their lifetime
Flaps
Flaps are permanent and never need to be replaced
Failure rate
Implants
FDA data shows that about 30% of implants are removed within 10 years
Flaps
Our practice performs DIEP flaps with a success rate of at least 99.5%
Breast consistency
Implants
Breasts reconstructed with implants typically feel firmer and cooler to the touch than normal body temperature
Flaps
Breasts reconstructed with natural tissue are soft and warm much like a natural breast
Breast sensation
Implants
Minimal to no return of sensation
Flaps
To a variable degree, sensation frequently returns
Surgery time
Implants
Mastectomy with implant reconstruction typically takes about 2-3 hours
Flaps
Mastectomy with DIEP flap reconstruction typically takes 3.5-5.5 hours
Hospital stay
Implants
Typical hospital stay is 1 night
Flaps
Typical hospital stay is 2-3 nights
Number of procedures
Implants
Two procedures are usually needed to complete the reconstruction, though sometimes it can be done in with just a single procedure
Flaps
Two procedures are usually needed to complete breast reconstruction using a woman’s own natural tissue
Recovery highlights
Implants
Most women can drive within 2 weeks of surgery and resume light exercise at 4-6 weeks
Flaps
Most women can drive within 2-3 weeks of surgery and resume light exercise at 4-6 weeks
Many women prefer the look and feel of natural-tissue breast reconstruction to implant breast reconstruction. In the hands of experienced surgeons like the ones on our team, natural-tissue reconstruction is performed with a degree of safety on par with that of breast implant reconstruction and with a flap success rate of about 99.5%. The main downside to a natural- tissue reconstruction is the need for a scar somewhere else on the body, at the site from which tissue is obtained. In the long term, natural tissue breast reconstruction provides life-long results associated with significantly fewer re-operations and failures than is the case with implant breast reconstruction. Nonetheless, for some women, breast implant reconstruction is the preferred approach.
Regardless of which method of reconstruction you prefer, we are here to help. With our team, you will be cared for by some of the most highly skilled and dedicated surgeons in the world. We have extensive experience with all methods of breast reconstruction and offer the full spectrum of breast reconstructive surgery to our patients.
Contact us to schedule an appointment or to learn more about which option may be right for you.
Learn more about the most sophisticated methods of natural tissue breast reconstruction
Timing of Breast Reconstruction Surgery

Timing of Breast Reconstruction Surgery
Once a woman has decided that she wants to have a breast reconstruction the next step is to decide on the best time to have the procedure.
Breast reconstruction performed at the same time as a mastectomy is called “immediate breast reconstruction” and reconstruction performed sometime after mastectomy is called “delayed breast reconstruction”. On occasion, a delayed breast reconstruction is performed within just a few weeks of mastectomy surgery, and is sometimes referred to as “immediate-delayed breast reconstruction.”
Each approach has specific advantages and disadvantages, and we will work with you to determine the optimal approach for your specific situation.
Immediate Breast Reconstruction
Immediate reconstruction allows a woman to wake up following a mastectomy with a reconstructed breast. For women who are candidates for skin-sparing mastectomy or nipple-sparing mastectomy, an immediate breast reconstruction generally offers the best possible aesthetic results. Immediate reconstruction preserves the greatest quantity of a woman’s own breast skin, minimizes scarring on the breast, and helps produce the best and most natural-looking results. In addition, immediate reconstruction will reduce the number of surgical procedures needed to treat a woman’s breast and reconstruct it, and reduce the total amount of time required for recovery and recuperation.
Although recent studies have shown that breast reconstruction surgery generally does not delay further cancer treatment (including chemotherapy and hormone therapy), your breast cancer surgeon or oncologist may recommend that reconstruction not be performed at the time of mastectomy.
If your postoperative treatment plan includes radiation therapy, we will generally recommend that natural tissue reconstruction be delayed until several months after radiation therapy is completed, however, we can often place an implant at the time of mastectomy to help preserve a maximal amount of a woman’s own breast skin and optimize the final aesthetic results.
Delayed Breast Reconstruction
Some women choose to delay breast reconstruction until sometime after mastectomy. Sometimes delaying reconstruction is done at the recommendation of the breast surgeon or oncologist. Other times women may wish to get out of the hospital as quickly as possible after mastectomy and opt to undergo a reconstruction at a more convenient time. Still others initially decide not to have reconstruction, but later decide they want to have a breast restored. And some women, not fully informed about their options for breast reconstruction prior to mastectomy, sadly, learn about reconstructive options only later.
In most cases, successful breast reconstruction can take place even after a delay of many years.
Delayed reconstruction can also be done for someone who is unhappy with a previous reconstruction. Women who are not satisfied with a previous natural tissue or implant reconstruction may elect to undergo a reconstruction well after the original procedure. Women who are dissatisfied with an implant reconstruction, for example, may decide to have their implants replaced or removed and replaced with their body’s own tissue.
Because the best and most reliable results of perforator flap breast reconstruction are typically obtained by surgeons who perform a high volume of this particular type of surgery, some women may choose to have a mastectomy with a breast surgeon in their local community and subsequently undergo reconstruction with a plastic surgeon who specifically specializes, as we do, in breast reconstruction surgery. Immediate-delayed breast reconstruction has a role in these and other situations. Of course, for women who live out of town and prefer to have an immediate breast reconstruction procedure, our staff can help plan an itinerary for consultation and, on the same visit, mastectomy and immediate reconstruction surgery in New York or Connecticut.
» Find out more about the timeline for breast reconstruction surgery
Shared Decision Making

Shared Decision Making
The ideal approach to breast reconstruction for one patient may not be the ideal for another. Individual circumstances, values, goals and preferences vary, and we believe these considerations must be incorporated into the decision-making process. That’s because every patient’s needs are different, and the right approach for breast reconstruction is not just about what is medically appropriate and reasonable.
Shared decision-making occurs when surgeons and patients work together to make decisions that are best for the patient. Optimal decisions account not only for evidence-based information about treatment options, but importantly, account for patient’s values and preferences.
There is no single “right” approach to breast reconstruction. Taking into account your preferences, needs, wants and expectations, and empowering you to actively participate in the breast reconstruction decision-making process, are critical elements for achieving the best possible outcomes.
Restoring Sensation After Mastectomy

Restoring Sensation After Mastectomy
Because most of the nerves that provide sensation to the skin and tissue of the breast travel directly within the breast tissue, removal of the breast by mastectomy unavoidably causes loss of sensation and numbness to the breast area. Women undergoing mastectomy should understand they will lose feeling in the area, regardless of whether they choose to have breast reconstruction or not. Women must also understand that nipple-preserving mastectomy preserves the physical structure of the nipple and areola, however the unique sensation associated with these structures is permanently lost following mastectomy.
Over a period of one to two years following mastectomy, some women experience return of some degree of sensation in the breast area, but for many patients minimal, if any, sensation ever spontaneously returns. Women who have natural tissue reconstruction generally experience a greater degree of sensation returning over time because nerve endings can grow within natural tissue, while implants represent a barrier to nerve growth.
Women who chose to have their breast reconstructed using their own tissue may be candidates for an additional procedure called "microneurorrhaphy.” Microneurorrhaphy connects a nerve in the tissue being used to restore the breast to a cut nerve at the mastectomy. This procedure, which is only possible with natural-tissue breast reconstruction, can improve the return of sensation to the breast. While it is not always possible to perform a microneurorrhaphy, when possible, we believe doing so helps to restore an important dimension of what having a breast reconstructed means.
Enhanced Recovery After Surgery: Recovering as Comfortably and Quickly as Possible

Enhanced Recovery After Surgery: Recovering as Comfortably and Quickly as Possible
The safety and comfort of our patients are our highest priorities.
To that end, our Enhanced Recovery After Surgery (ERAS) protocol means patients are able to undergo surgery with less pain and faster recoveries than ever before. Gone are the days of “nothing to eat or drink after midnight” and the need for a load of narcotic painkillers after surgery.
We use a multipronged approach to help minimize your pain, help you avoid nausea, vomiting, or constipation, and to facilitate a rapid return to your usual activities.
Our protocol includes allowing most patients to drink clear liquids, including black coffee, up to 3 hours ahead of surgery. We administer medications that reduce pain, anxiety and nausea even before you enter the operating room. While you are asleep, our anesthesia team will continue to administer medications that have the same effect. During surgery, we deliver long-acting local anesthetics (nerve blocks) near the surgical sites to block pain pathways so that you can wake up comfortable and remain comfortable without the need for much, if any, narcotic or opioid painkillers.
Because our enhanced recovery protocol is so effective, most of our patients are able to recovery comfortably using little or no narcotic/opiate pain medication after surgery. Most women who opt for an implant reconstruction stay just overnight, and those who opt for a natural tissue reconstruction stay just 2 or 3 nights in the hospital before going home.Dr. Greenspun has been a pioneer in bringing ERAS pathways to the hospitals at which he operates, and has given numerous presentations at medical meetings and conferences on the benefits that such interventions provide. Ahead of surgery, you will be provided with specific instructions for the ERAS protocol that is right for you.
Correcting Botched Breast Reconstruction

Corrective Breast Reconstruction
Using sophisticated and innovative techniques, we usually find that it is possible to substantially improve upon, or even correct, most unsatisfactory results or previous reconstructive failures. This has been our experience, even for women who have previously been told by other doctors that there is little or nothing that could be done for them.
Common issues that we address include:
- Unsatisfactory or inadequate overall appearance, contour or symmetry
- Drooping or sagging of natural tissue reconstruction
- Reconstructed breasts that are too small or too large
- Implant complications such as capsular contracture, rippling or a shift in the position of an implant
- Pain and discomfort
- Chest or arm stiffness
- Complete failure of a prior reconstruction
- Radiation related problems
Corrective breast surgery is often challenging, and every situation requires a unique solution. Taken together, our experience and comprehensive skill set allow us address each situation using a wide range of techniques –from simple approaches such as implant revision, to the most advanced microsurgical procedures performed anywhere in the world.
If you are unhappy with your breast reconstruction, feel like your breast reconstruction may have been “botched” or have had a breast reconstruction failure, we may be able to help improve your results and enhance your quality of life.
Click here to see some examples of how we have been able to help women with prior breast reconstructions that they felt were unsatisfactory.
Breast Reconstruction Timeline

Breast Reconstruction Timeline
With a few exceptions, regardless of the type of reconstruction selected, two surgical procedures or “stages” will likely be needed to complete your full breast reconstruction. In some cases, however, you may be able to have the reconstructive process completed in a single operation.
Surgery may include nipple reconstruction as well as a procedure on the unaffected breast to produce symmetry. While the majority of women prefer to have nipples reconstructed as this minor procedure greatly enhances the aesthetic results and the natural appearance of their reconstructed breast, not all women choose to do so.
Our practice offers breast reconstruction surgery in Connecticut and New York City. If you live outside of these areas, you can comfortably return home between stages of treatment.
PROCEDURE-SPECIFIC TIMELINES
Below, you will find timelines that are typical for each type of breast reconstruction that the surgeons of the Advanced Reconstructive Surgery Group offer. Depending on individual patient circumstances, the time course to complete reconstruction may vary.
MICROSURGICAL PERFORATOR FLAP BREAST RECONSTRUCTION:
STAGE I: Creating a Breast with Natural Tissue
At the first stage of natural-tissue breast reconstruction, transferring borrowed tissue to the mastectomy site restores a breast. The tissue is sculpted to restore the natural shape and form of the breast as closely as possible. Women who undergo this type of surgery generally stay three nights in the hospital for monitoring, but typically have minimal pain.
STAGE II: Refining Your Breast Reconstruction And Nipple Reconstruction
About three months or more after the first stage of reconstruction, a relatively short outpatient procedure can be done to refine the shape of your reconstructed breasts, and to reconstruct nipples, if that is part of the surgical plan. You’ll be able to go home the same day as this procedure and most women can return to work or other non-vigorous activities after only a few days. The shape of your reconstructed breasts will be carefully refined, as will the donor the donor site, to achieve the best possible aesthetic results. If you have had only one breast reconstructed, a breast lift, breast augmentation or breast reduction can be done on the unaffected breast at this time to improve symmetry.
To learn more about natural tissue reconstruction, click here
ONE-STAGE BREAST IMPLANT RECONSTRUCTION
Direct-to-Implant reconstructions, also called “One-Step Reconstructions,” or “One-Stage Reconstructions,” are generally our preferred, and our patients’ preferred approach to breast implant reconstruction. That’s because when it is possible to perform such procedures, at the same surgery, an implant can be placed directly in the space created by the mastectomy, and therefore there is no need to undergo tissue expansion. Furthermore, the potential for chronic problems—including discomfort, reduced strength, and reduced mobility—associated with lifting of the chest wall muscles in the more traditional tissue expander-implant approach, is dramatically reduced. Women who have a one-stage breast implant reconstruction generally go home the day after surgery.
TISSUE EXPANDER/IMPLANT RECONSTRUCTION
STAGE I: Creating Space for a Breast Implant by Tissue Expansion
A tissue expander will be placed under the pectoralis muscle of the chest, typically at the time of a mastectomy. In the weeks following surgery, by injecting sterile fluid or air at a series of office visits, the expander will be gradually enlarged in order to expand the tissue at the mastectomy site to make room for an implant.
STAGE II: Replacing a Tissue Expander with a Breast Implant
Following completion of the expansion process, at a second surgery approximately 4-12 weeks following the initial procedure, the tissue expander is exchanged for a breast implant. A nipple reconstruction can sometimes be done at this stage, but often it is done during a short additional procedure. You’ll be able to go home the same day as this procedure and most women can return to work or other non-vigorous activities after only a few days. If you have had only one breast reconstructed, a breast lift, breast augmentation or breast reduction can be done on the unaffected breast at this time to improve symmetry.
To learn more about tissue expander/implant reconstruction, click here
TATTOO: RESTORING COLOR TO YOUR RECONSTRUCTED NIPPLE AND AREOLA
Natural appearing color can be restored to reconstructed nipples and areole (the pigmented area that surrounds the nipples) about three months after nipple reconstruction. Pigment is applied as a 3-D medical tattoo in the comfort and privacy of our office. If necessary, topical numbing medication can be used to assure that the tattooing is painless.
Breast Reconstruction After Mastectomy

Breast Reconstruction After Mastectomy
All breast reconstruction procedures fall into one of two broad categories:
- Breast reconstruction using natural tissue from your own body
- Breast reconstruction using breast implants
Natural tissue generally provides the most natural-appearing (and feeling) as well as most durable type of breast restoration. Reconstruction with breast implants, however, may be preferred by some women, especially if they want to avoid a scar on a location other than the breast/s.
The surgeons of our Advanced Reconstructive Surgery Group specialize breast reconstruction surgery.
STATE-OF-THE-ART APPROACHES TO BREAST RECONSTRUCTION
NATURAL TISSUE
Living tissue that is surgically relocated from one part of the body to another is called a “flap.” The most advanced methods of natural-tissue breast reconstruction, known collectively as perforator flaps, use natural tissue to restore a breast without compromising a woman’s muscles in the process. These procedures can be performed with a minimal amount of pain. They typically result in a reconstructed breast that is warm, soft and forever part of a woman’s body. Our practice has roughly a 99.5% success rate for these procedures. Because perforator flaps do not remove muscle, these procedures are now considered by many experts to be the gold standard for natural-tissue breast reconstruction.
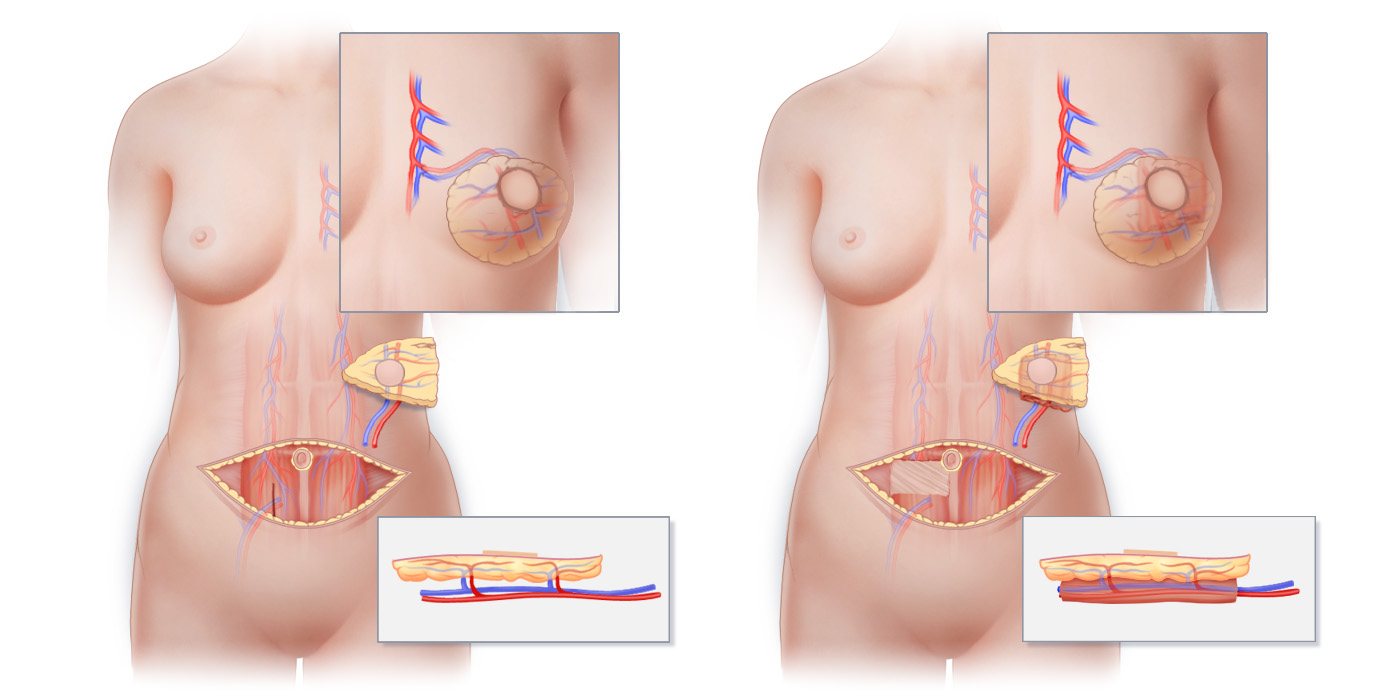
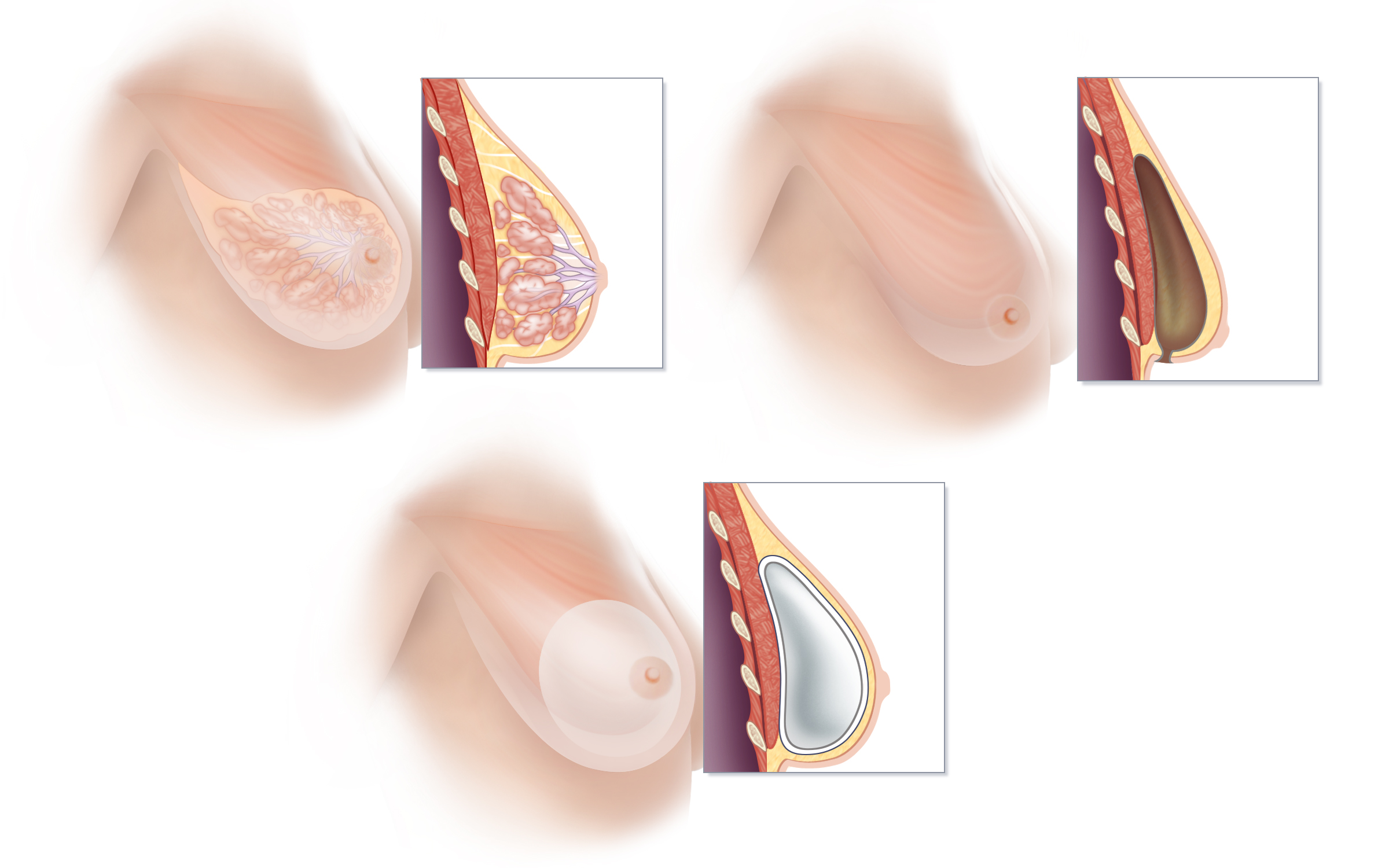
One of the most important factors differentiating the various methods of natural-tissue breast reconstruction from one another is whether or not muscle is surgically removed from the site from which the tissue is borrowed. Perforator flaps such as the deep inferior epigastric perforator flap (DIEP flap) preserve muscle, while musculocutaneous flaps such as the free transverse rectus abdominus myocutaneous flap (free TRAM flap) sacrifice important muscles. (A) Preparation of a DIEP flap takes place without removing any muscle from the abdomen. (B) Preparation of a free TRAM flap requires removal of rectus abdominus muscle from the abdomen. It is important to note that muscle does not ever grow back, so operations that remove muscle produce life-long change. Lower insets show flaps in cross-sectional view.
One of the most important factors differentiating the various methods of natural-tissue breast reconstruction from one another is whether or not muscle is surgically removed from the site from which the tissue is borrowed. Perforator flaps such as the deep inferior epigastric perforator flap (DIEP flap) preserve muscle, while musculocutaneous flaps such as the free transverse rectus abdominus myocutaneous flap (free TRAM flap) sacrifice important muscles. (A) Preparation of a DIEP flap takes place without removing any muscle from the abdomen. (B) Preparation of a free TRAM flap requires removal of rectus abdominus muscle from the abdomen. It is important to note that muscle does not ever grow back, so operations that remove muscle produce life-long change. Lower insets show flaps in cross-sectional view.
BREAST IMPLANTS
For women who opt to have breast reconstruction using breast implants, it is now sometimes possible to place a breast implant directly into the space created by the mastectomy, just underneath the skin of the breast. While this state-of-the-art approach is not suitable in every situation, it is often preferred over the traditional approach of tissue expander/breast implant reconstruction that involves surgical disruption of the muscles of the chest that can be painful in the short term, and may compromise muscle function and be uncomfortable in the long term. Unfortunately, breast implants generally do not last forever. The advantages of this quicker initial surgery should be weighed against the frequency with which later complications occur, such as capsular contracture, implant rupture and a high rate of unplanned re-operation.
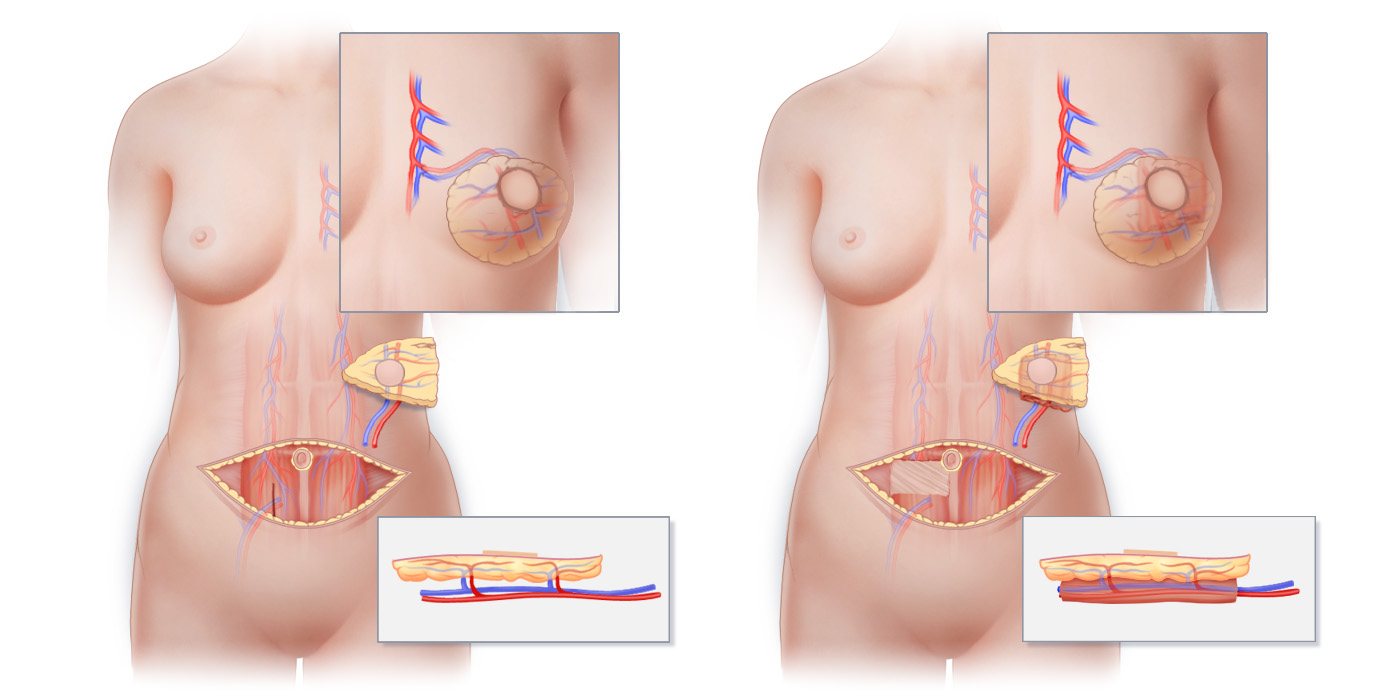
We perform a state-of-the-art method of implant reconstruction that preserves the pectoralis muscle of the chest in its natural form and places a breast implant into the same location that breast tissue is found (A). This method, known as prepectoral breast implant reconstruction, takes advantage of the space created by the removal of breast tissue at the time of mastectomy (B) to achieve a reconstruction without disrupting the pectoralis muscle. By placing a silicone-filled implant wrapped in specialized acellular dermal matrix directly into the space that results at the time of mastectomy (C), weakness and discomfort associated with traditional breast implant reconstruction (in which an implant is placed beneath the pectoralis muscle) is avoided. Additionally, with prepectoral breast implant reconstruction, the unsightly movement of implants known “animation deformity,” frequently seen with physical activity in women who have had traditional breast implant reconstruction, is avoided.
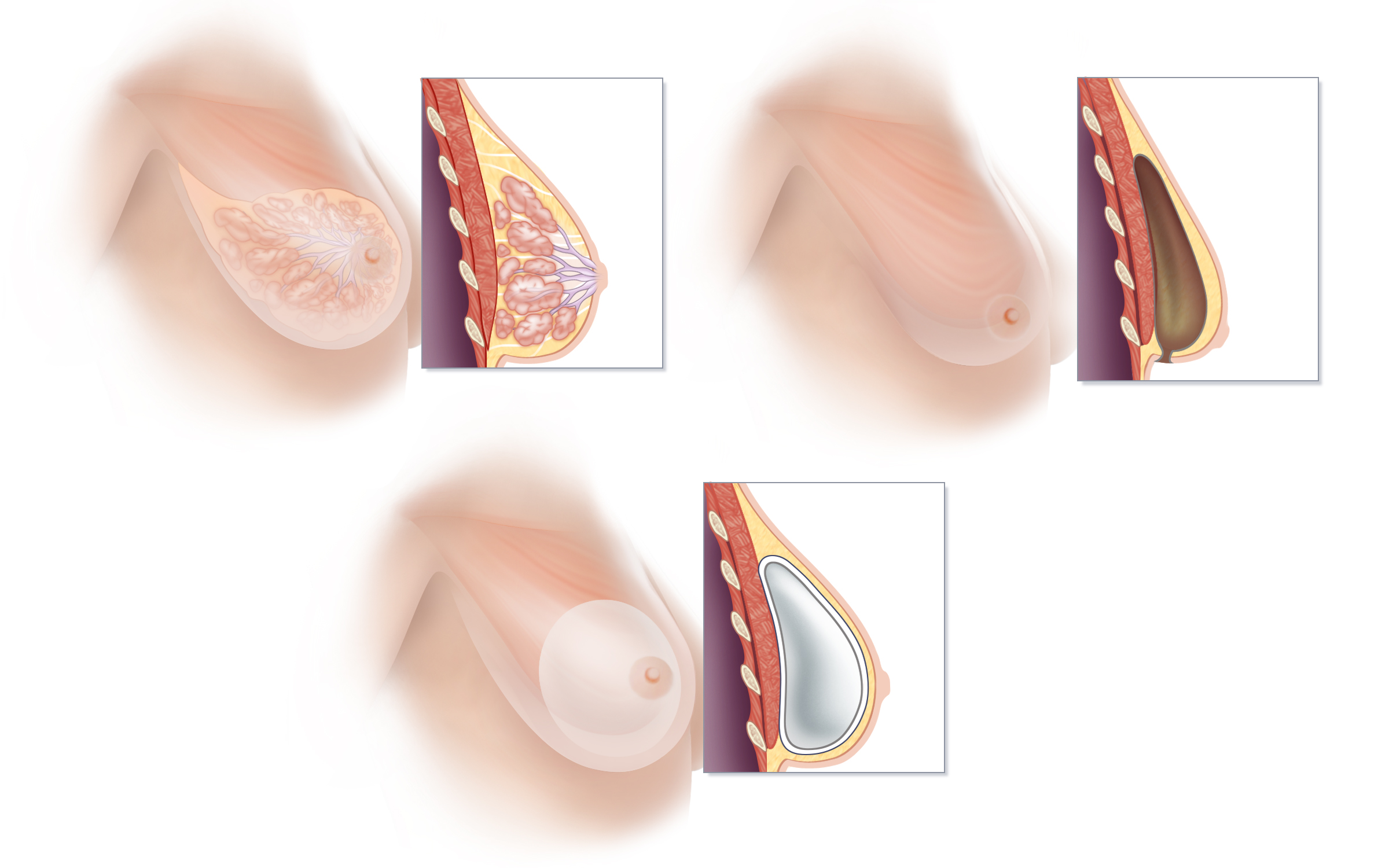
We perform a state-of-the-art method of implant reconstruction that preserves the pectoralis muscle of the chest in its natural form and places a breast implant into the same location that breast tissue is found (A). This method, known as prepectoral breast implant reconstruction, takes advantage of the space created by the removal of breast tissue at the time of mastectomy (B) to achieve a reconstruction without disrupting the pectoralis muscle. By placing a silicone-filled implant wrapped in specialized acellular dermal matrix directly into the space that results at the time of mastectomy (C), weakness and discomfort associated with traditional breast implant reconstruction (in which an implant is placed beneath the pectoralis muscle) is avoided. Additionally, with prepectoral breast implant reconstruction, the unsightly movement of implants known “animation deformity,” frequently seen with physical activity in women who have had traditional breast implant reconstruction, is avoided.
Connecticut Breast Reconstruction New York Breast Reconstruction
Breast reconstruction surgery can restore the shape, size and appearance of a woman’s breast following mastectomy or lumpectomy. New kinds of treatment and improved reconstructive surgical techniques mean that women who have breast cancer today have more and better options than ever before. Dr. Greenspun is a top breast reconstruction specialist; his offices are located in Connecticut and New York.
» Contact us for information about breast reconstruction in Greenwich, Connecticut, New York and New Jersey.
To learn more about breast implant reconstruction, click here
To learn more about natural tissue reconstruction, click here
Corrective Breast Reconstruction

Corrective Breast Reconstruction
Our expertise, experience and broad spectrum of reconstructive surgical capabilities allow us to help women who have experienced reconstructive failure, unsatisfactory results, or chronic pain from previous breast reconstruction surgery. It is not necessary to live with pain or disfigurement from prior surgery.
If you are unhappy with your breast reconstruction, feel that your breast reconstruction may have been done inadequately, or have had a breast reconstruction failure, we may well be able to help.
Using sophisticated and innovative techniques, we can often considerably improve upon, or even correct, unsatisfactory results or previous reconstructive failures. This has been our experience even for women who have previously been told by their doctors that there is little or nothing that could be done for them.
Common issues that we address include: pain, scarring, implant complications, capsular contracture, objectionable shape, chest or arm stiffness, poor symmetry, complete failure, and radiation-related problems.
Corrective breast surgery is often challenging. Our experience and fully comprehensive skill set allow us to address each situation using a wide range of techniques––from simple approaches such as implant revision to the most advanced microsurgical procedures performed anywhere in the world.
Click here to see examples of women with previous unsatisfactory reconstructions who we were able to help.
About Dr. Lamelas

About Dr. Lamelas
Breast Reconstruction Specialist - New York and Connecticut
Dr. Andreas M. Lamelas is a Harvard fellowship trained Plastic Surgeon, board certified by the American Board of Plastic Surgery, with a focus on natural tissue breast reconstruction and surgical treatment for breast cancer related lymphedema. He received a Bachelor of Science degree in Biomedical Engineering at the University of Virginia, graduating with Honors. He then went onto receive his Medical Degree at Temple University School of Medicine where he was one of four students to be selected for early membership to the Alpha Omega Alpha Honor Society. Dr. Lamelas completed his Plastic Surgery Residency at the Icahn School of Medicine at Mount Sinai in Manhattan and was selected to serve as Chief Resident. He then went on to Harvard Medical School to complete a highly-competitive Fellowship in Microsurgery at Beth Israel Deaconess Medical Center.
Dr. Lamelas and his wife, Brooke, live in Connecticut and are avid travelers. In his free time, he enjoys photography, tennis, exploring new restaurants and relaxing with a good book. In addition to breast reconstruction, he is interested in body contouring, reconstruction for skin cancer and aesthetic surgery of the face and body.
Dr. Lamelas is dedicated to the progression of the field of Plastic Surgery, publishing numerous peer-reviewed articles and book chapters as well as presenting at national academic conferences. He strives to establish trusting patient relationships and achieve the best results for each one of his patients.
» Contact us if you would like to make an appointment and learn more about your options


» Contact us if you would like to make an appointment and learn more about your options
Perioperative Instructions

Day Before Surgery
● Eat a regular dinner; drink 12-16oz of gatorade prior to bed
● Shower with hibiclens soap (can be purchased at any retail pharmacy) the night before surgery, do not scrub markings and darken faded markings with sharpie as needed
● Do not shave any body hair the night before or morning of surgery as this increases the risk of post-operative infection
● Nothing to eat or drink after midnight unless otherwise directed
Morning of Surgery
● Take one pill of Emend 40 mg (prescription given during pre-op appointment) with 12 oz of gatorade 3 hours prior to your expected surgery start time (start time will be provided the day before surgery). Finish the 12-16oz of gatorade within 15 minutes
● If you are a consistent coffee or tea drinker, you may have one cup of black coffee or plain tea at least 3 hours prior to surgery
● Shower with hibiclens soap. Do not apply any moisturizers, skin treatments or deodorant the morning of surgery.
After Surgery
● Pain after surgery is managed first with non-narcotic analgesia (Tylenol and Ibuprofen). Please have Tylenol 650 mg and Ibuprofen 800 mg available at home prior to surgery. Specific instructions on when to take these medications will be provided.
● A prescription for 5 pills of oxycodone 5 mg will be given at the pre-op appointment and should only be taken if absolutely necessary.
● Use anti-nausea medication as needed. A prescription for either Zofran or Reglan will be given during pre-op appointment.
● Once permitted to shower, use hibiclens soap for two weeks after surgery.
● Specific instructions regarding dressing and drain care will be provided prior to discharge home.
Breast Reconstruction Surgery

Breast Reconstruction Surgery
Breast reconstruction restores the form of a woman’s breasts, and not surprisingly, countless studies have demonstrated important emotional and psychological benefits for women who choose to have breast reconstruction surgery following mastectomy. Nevertheless, the decision to have a breast reconstructed after mastectomy is a very personal one.
Our team of compassionate experts is here to support you and your family, before, during and after surgery. Our highly specialized practice is devoted to the most innovative and advanced methods of breast reconstruction surgery. During the past decade and a half, we have successfully performed well over 1,000 perforator flap breast reconstructions, including DIEP flaps, stacked DIEP flaps, multi-flap reconstructions, SIEA flaps, SGAP flaps, LAP flaps, and PAP flaps. We also regularly perform breast reconstruction using breast implants because we recognize that different approaches are beast for different patients. Our expertise, comprehensive approach, proven track record, and highly personalized care set us apart.
If you are thinking about breast reconstruction surgery, you may wish to consider these important questions:
- Do the advantages of having breast reconstruction appeal to you?
- If you choose to have a breast reconstructed after mastectomy, what type of breast reconstruction best suits your particular goals?
- What kind of results can I reasonably expect?
- When should your reconstruction be done - At the same time as the mastectomy (immediate breast reconstruction -link), or any time after mastectomy (delayed breast reconstruction - link)?
- Should I consider surgery on my other breast to help them match after reconstruction?
- Who should perform the reconstructive surgical procedure?
- How many of these procedures have your plastic surgeon done?
- How long will it take to recover?
Choosing a breast reconstruction option can feel overwhelming. Each method of reconstruction has its own benefits and risks. Understanding the specifics of different techniques can help you feel more secure as you make an informed decision about the kind of breast reconstruction that will be best for you.
Learn more about our procedures:
Breast reconstruction procedures can be grouped into two broad categories:
Recovery After Breast Reconstruction Surgery

RECOVERY AFTER BREAST RECONSTRUCTION SURGERY
While no two people experience precisely the same path to full recovery, this overview will suggest what you can typically expect to experience after surgery. We hope that this information helps you to plan for your recovery.
RECOVERING AFTER PERFORATOR-FLAP Breast Reconstruction
Most patients do not have considerable pain following flap surgery. In fact, most patients need little, if any, narcotic medication following perforator-flap breast reconstruction surgery.
DURING YOUR HOSPITAL STAY
Right after surgery…
You will be brought to the recovery room, where your nurse will make sure you’re comfortable and will check on you and closely monitor your surgical site. If you like, you can have family or others visit with you in the recovery room.
During your hospital stay…
From the recovery room you will be taken to a comfortable private room where you will have personal nursing care for the first 24 hours of your recovery. You’re welcome to have someone stay overnight with you in your hospital; a fold-out bed for a guest will be available right in your room. You will be able to shower in the hospital. Most patients spend 3 nights recuperating before going home, though some can return home even sooner.
AFTER YOU LEAVE THE HOSPITAL
The first few weeks at home…
While you may feel tired and a bit sore in the first few weeks following surgery, most women do not have significant pain. You may feel comfortableusing just over-the-counter pain relievers, such as acetaminophen or ibuprofen.
While you cannot participate in vigorous or strenuous activity for several weeks after surgery, you will be able to take walks, work at a desk, climb stairs and engage in other non-strenuous activity as soon as you leave the hospital. Most women can resume driving a car sometime between the 2nd and 3rd week after surgery. Most women can return to light aerobic activity about 4 weeks after surgery, and most will be able to resume full physical activity 6 to 8 weeks after surgery. Dr. Greenspun will advise you, based upon how you are recovering, when it is safe to resume various activities.
Returning to work…
Since recovery time from surgery will vary from person to person, it is not possible to predict exactly how soon after surgery you will be able to return to work. We generally recommend taking 3-4 weeks off from work. Some women are able to return to work sooner, and some may take a little longer especially if their work is physically demanding.
RECOVERING AFTER BREAST IMPLANT RECONSTRUCTION
In most cases, a woman will spend one night in the hospital following mastectomy and placement of an implant or tissue expander.
Following the placement of a tissue expander or implant, you can expect to experience some muscle soreness and spasm, particularly if an expander or implant is placed behind or under your muscle. The process of tissue expansion begins about one and a half weeks or more after surgery. Every 1-2 weeks, during a short office visit, sterile fluid will be injected through the overlying skin into the tissue expander, in order to gradually create space for an implant.
Your upper back and shoulder may also be sore during this process. It is often helpful to do gentle range-of-motion exercises to avoid shoulder stiffness, and you will receive specific instructions from Dr. Greenspun about what you can and cannot do. As is also the case with flap reconstruction, you will not be able to participate in vigorous or strenuous activity for 6 to 8 weeks following surgery; you will be able to take walks, work at a desk, climb stairs and engage in other non-strenuous activity as soon as you leave the hospital. Many women are able to return to light aerobic activity about 4 weeks after surgery, and most are allowed to resume full physical activity 6 to 8 weeks after surgery. We generally recommend taking 2-3 weeks off from work, though some women may require a bit more time.
Repair of Unsatisfactory or Failed Breast Implants

Repair of Unsatisfactory or Failed Breast Implants
Whether placed for cosmetic breast augmentation or for breast reconstruction, unfortunately, implants can cause problems or not look and feel as one wants them to. Whether an unsatisfactory or failed implant breast reconstruction is the result of a “botched” breast surgery, or issues inherent to the use of breast implants, there are options to correct or considerably improve even the most disappointing results. We have helped a large number of women who felt devastated because they had previously been told there was nothing more that could be done to improve a disappointing result or relieve chronic pain.
Revising Unsatisfactory Breast Implant Reconstruction
The goal of breast implant reconstruction revision is to improve the overall look and feel of a previous implant breast reconstruction. Revision may be desired when an initial effort at reconstruction was simply unsatisfactory, or because an initially acceptable breast implant reconstruction changed over time. Animation or dynamic deformity—when the breasts move unnaturally with physical activity—is another reason many women seek implant revision surgery. Breast implant revision surgery is not a single or standard procedure but a precisely tailored surgical procedure developed specifically to account for a patient’s preexisting anatomy, her goals and objectives.
Revision reconstruction often includes one or more of the following:
- Removal of an implant or implants and replacement with the newer generation implant and/or implants of a different size
- Reshaping of the “pocket” that hold the implant
- Changing the position of an implant from “below the muscle” to a position “above the muscle”
- Fat grafting
- Lifting the breast
Replacing Implants with your Body’s Own Tissue
For women who no longer wish to live with implants or who have already had an implant removed, breast reconstruction with one’s own tissue can be an excellent option. Many women who have had discomfort with their breast implants report significant reduction in breast pain, and even the elimination of breast pain altogether, after their implants are removed and replaced with natural tissue. Studies have repeatedly shown that radiation increases the risk of complications and poor aesthetic outcomes for women who have implant-based breast reconstruction. Our experience mirrors that reported in the medical literature, so in our practice, for women who have had radiation as part of their treatment, we almost always suggest replacing an unsatisfactory implant reconstruction with a natural-tissue breast reconstruction.
» Learn more about sophisticated natural-tissue alternatives to breast implant reconstruction
» Contact us if you would like to make an appointment and learn more about your options
A Word About Breast Implants - Breast Implants Do Not Last Forever
Problems with breast implants are not unusual, and rarely do they reflect underlying issue with a person’s overall health or body.
A common myth suggests that breast implants need to be changed every ten years. While there is no need to routinely remove and replace breast implants regardless of how long they have been in a person’s body, problems with implants that require additional surgery including implant removal, occur increasingly the longer an implant has been in place. Though almost never life threatening, amongst the problems leading to unplanned surgery are: ruptures, deflations, capsular contracture, infection, implant migration, pain, unnatural or unsatisfactory appearance, rippling and asymmetry.
Data collected on breast implants by the Food and Drug Administration shows:
- About 1 out of every 3 women who undergo breast reconstruction with implants will need additional unplanned surgery within just 3 years; the chances of needing additional surgery rise to over 50% within about 10 years.
- About 1 of every 3 women who have a breast implant reconstruction will experience a problem that requires that her implants be removed (with or without replacement of the implant) within 10 years of their initial surgery.
The FDA has several excellent publications on their website highlighting the more common problems that occur in the breast or chest area following implant placement; these include photographs documenting implant complications.
- Breast Implant Consumer Information
- Breast Implants - Potential Local Complications and Reoperations
- Photographs and/or Illustrations of Breast Implant Complications
The Thigh As A Donor Site: PAP, DUG and TUG Flaps

PAP Flap, DUG Flap and TUG Flap
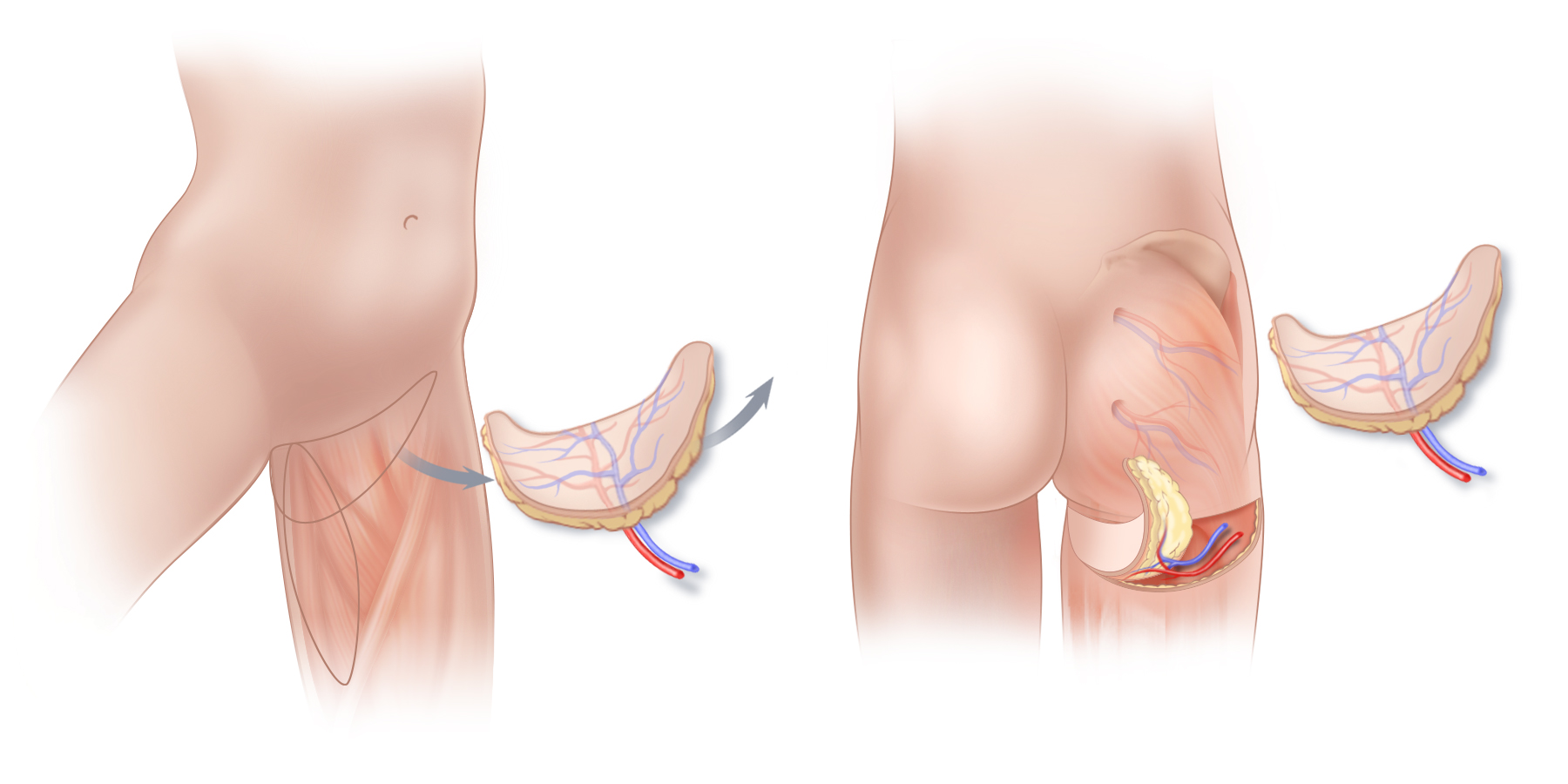
Tissue from the upper thigh can be used for natural-tissue breast reconstruction. (A) the Transverse Upper Gracilis or TUG flap, and the Diagonal Upper Gracilis or DUG flap may be good options when excess tissue is present on the inner thigh. Although technically TUG and DUG flaps are not perforator flaps, TUG/DUG flaps remove only a small piece of muscle from the inner thigh, an area of the body with a very large muscle mass, and thus weakness and functional impairment are avoided. (B) Tissue from the back of the upper thigh (PAP Flap) can also be used for natural-tissue breast reconstruction. The scar that results following a PAP flap procedure will vary from person to person as the anatomy of the blood vessels in this portion of the thigh is quite variable.
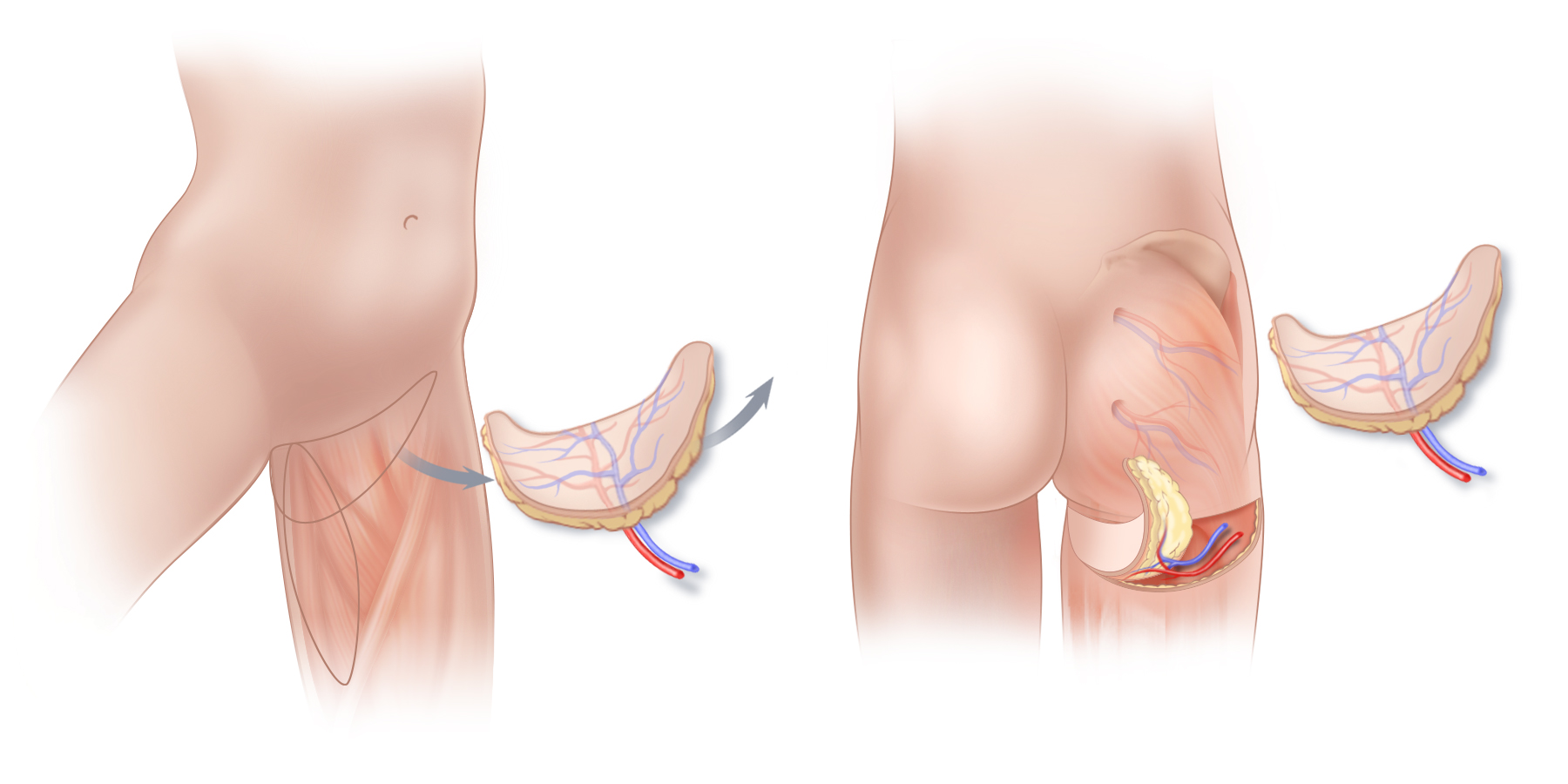
Tissue from the upper thigh can be used for natural-tissue breast reconstruction. (A) the Transverse Upper Gracilis or TUG flap, and the Diagonal Upper Gracilis or DUG flap may be good options when excess tissue is present on the inner thigh. Although technically TUG and DUG flaps are not perforator flaps, TUG/DUG flaps remove only a small piece of muscle from the inner thigh, an area of the body with a very large muscle mass, and thus weakness and functional impairment are avoided. (B) Tissue from the back of the upper thigh (PAP Flap) can also be used for natural-tissue breast reconstruction. The scar that results following a PAP flap procedure will vary from person to person as the anatomy of the blood vessels in this portion of the thigh is quite variable.
The skin and fat of the upper thigh can be used to reconstruct breasts with a natural appearance using warm, supple, living tissue. The Profunda Artery Perforator flap or PAP flap, the Transverse Upper Gracilis or TUG flap, and the Diagonal Upper Gracilis or DUG flap can be good options for breast reconstruction for some women. The shape of these flaps facilitates the sculpting of breasts with especially youthful projection and contour. However, because PAP flaps, DUG flaps, and TUG flaps generally produce a scar on the upper thigh that is not well-hidden by a bathing suit, and because these flaps can sometimes result in a change in thigh and lower buttock contour that is unfavorable, PAP, DUG and TUG flaps are generally used in our practice, only when other, more favorable donor sites are not an option.
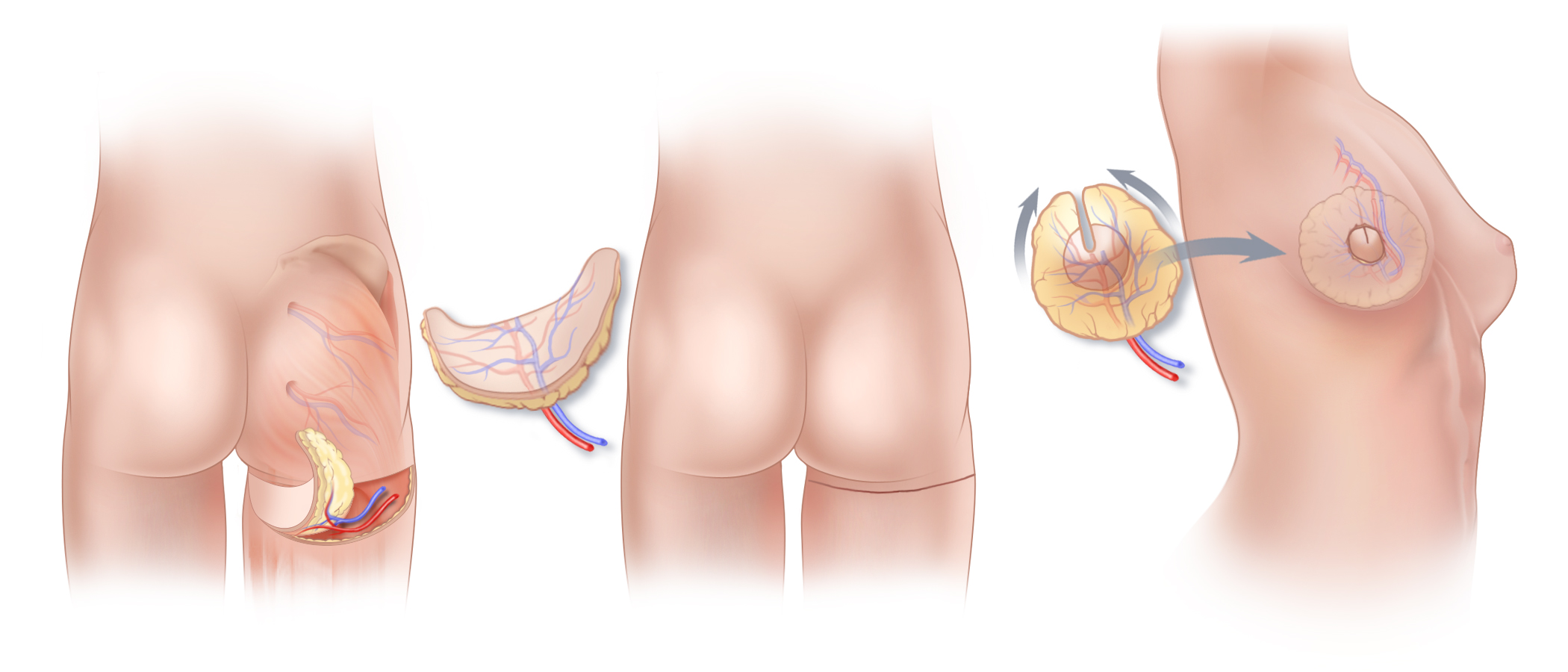
Tissue from the upper part of the thigh can be used for natural-tissue breast reconstruction. (B) The scar that results following a PAP flap procedure lies on the back of the thigh, ideally just below the lower buttock crease, but often lower down. The scar typically extends somewhat onto both the inner and outer thighs. (C) Similar to the way in which TUG and DUG flaps are shaped to reconstruct a breast, by bringing the ends of the PAP flap together, the crescent-shaped flap is formed into a reconstructed breast with youthful contours and projection. The flap is transferred to the chest, and the blood vessels of the PAP flap are connected to blood vessels at the chest using microsurgical techniques. The location of the surgical scar on the breast will depend on the technique used for the mastectomy itself.
Tissue from the upper part of the thigh can be used for natural-tissue breast reconstruction. (B) The scar that results following a PAP flap procedure lies on the back of the thigh, ideally just below the lower buttock crease, but often lower down. The scar typically extends somewhat onto both the inner and outer thighs. (C) Similar to the way in which TUG and DUG flaps are shaped to reconstruct a breast, by bringing the ends of the PAP flap together, the crescent-shaped flap is formed into a reconstructed breast with youthful contours and projection. The flap is transferred to the chest, and the blood vessels of the PAP flap are connected to blood vessels at the chest using microsurgical techniques. The location of the surgical scar on the breast will depend on the technique used for the mastectomy itself.
The PAP, TUG and DUG flaps are similar to one another, in that they all come from the upper thigh. The technique and resultant scar vary from one flap to another, and the distribution of fatty tissue on an individual’s upper thigh will play a role in determining which of these flaps is best suited for her. The PAP flap uses tissue from the back of the thigh, whereas the TUG and DUG flaps take tissue from the inner thigh. While the PAP flap is a true perforator flap, and therefore does not take any muscle from the donor site, DUG and TUG flaps require that a small amount of gracilis muscle be incorporated into the flap to assure the adequacy of blood flow. However, since the gracilis muscle is a very small muscle (unlike the rectus abdominis muscle on the abdomen), and not one of the primary muscles of the leg, it is generally not missed after TUG or DUG flap breast reconstruction surgery, and there is no risk of developing a hernia at the donor site.
TUG Flap, PAP Flap and DUG Flap Surgery in Connecticut and New York
Please Contact us if you would like more information about TUG flap, DUG flap or PAP flap breast reconstruction, or information about other options for breast reconstruction including DIEP flap surgery after mastectomy. Our practice has offices in New York and Greenwich, Connecticut.
SGAP & IGAP Flaps

Superior Gluteal Artery Perforator & Inferior Gluteal Artery Perforator Flaps
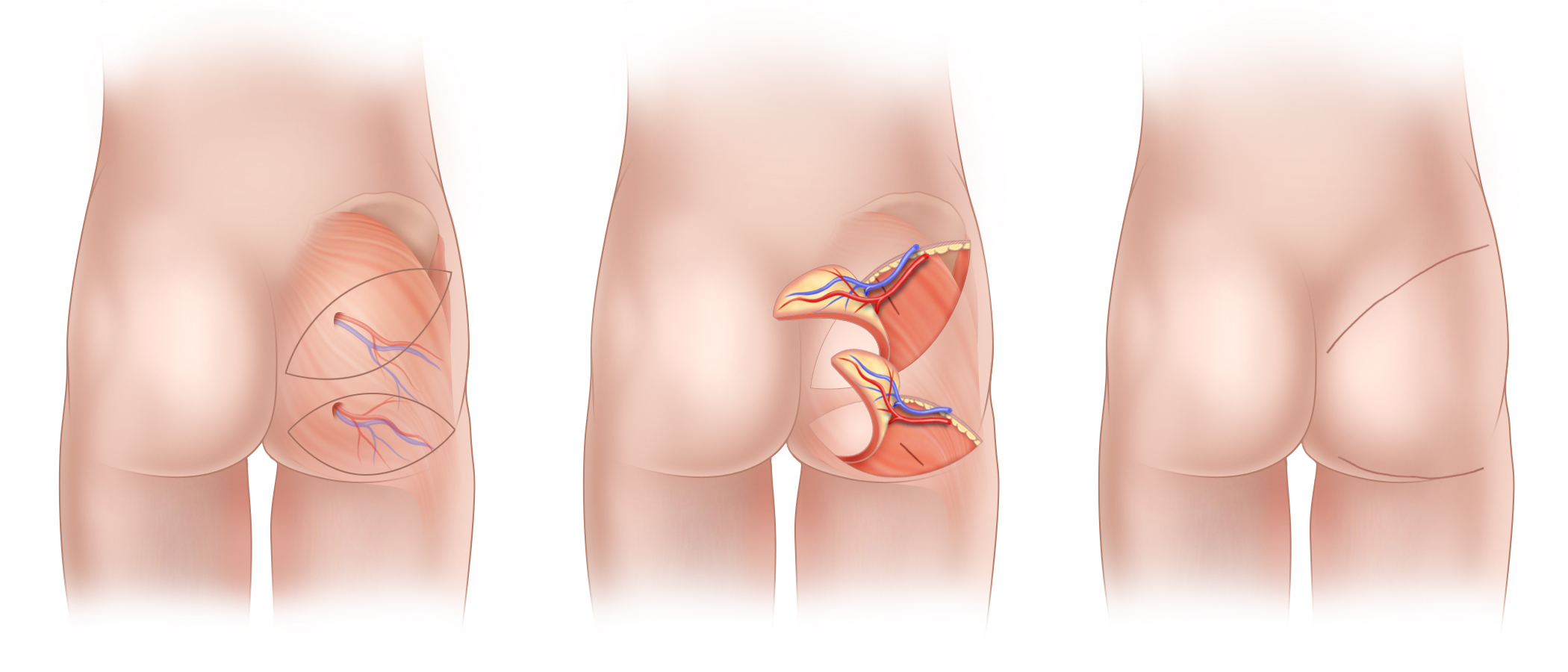
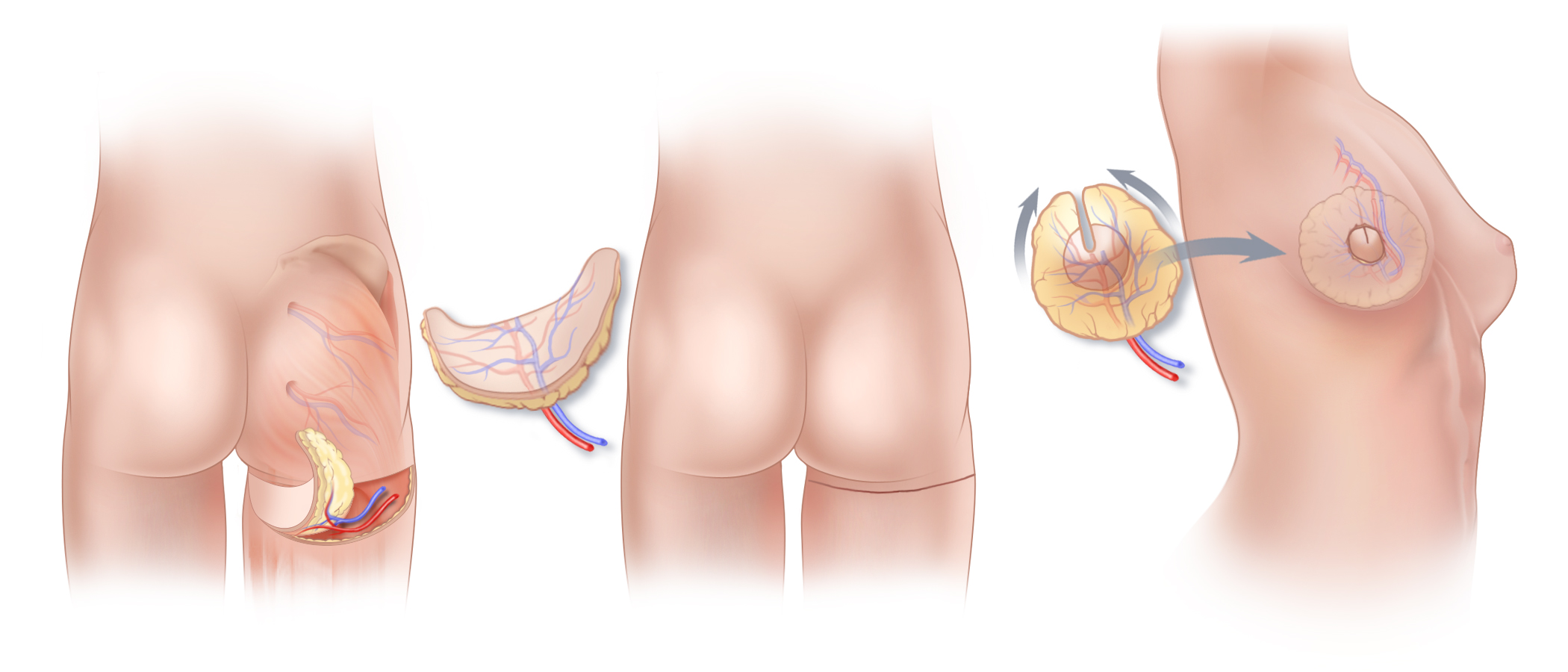
(A)The superior gluteal artery and vein provide the blood supply to the skin and fatty tissue of the upper buttock while the inferior gluteal artery and vein supply the skin and fatty tissue of the lower buttock. These vessels can be used to create a superior gluteal artery perforator (SGAP) flap from the upper buttock, and an inferior gluteal artery perforator (IGAP) flap from the lower buttock tissue. (B) Both SGAP and IGAP flaps are shown being surgically elevated from the buttock; with either flap, the gluteal muscles are left intact at the donor site. (C) The scars that result from harvest of SGAP and IGAP flaps are generally well concealed in clothing. Nonetheless, because harvest of these flaps can cause unfavorable contour changes at the buttock, we seldom perform these procedures any longer, and instead, favor alternatives such as the lumbar artery perforator flap (LAP).
(A)The superior gluteal artery and vein provide the blood supply to the skin and fatty tissue of the upper buttock while the inferior gluteal artery and vein supply the skin and fatty tissue of the lower buttock. These vessels can be used to create a superior gluteal artery perforator (SGAP) flap from the upper buttock, and an inferior gluteal artery perforator (IGAP) flap from the lower buttock tissue. (B) Both SGAP and IGAP flaps are shown being surgically elevated from the buttock; with either flap, the gluteal muscles are left intact at the donor site. (C) The scars that result from harvest of SGAP and IGAP flaps are generally well concealed in clothing. Nonetheless, because harvest of these flaps can cause unfavorable contour changes at the buttock, we seldom perform these procedures any longer, and instead, favor alternatives such as the lumbar artery perforator flap (LAP).
Although the abdomen (DIEP flap), flanks (Extended DIEP flap) and lumbar region (LAP flap) are generally first choices for perforator-flap breast reconstruction, not every women is a good candidate for a flap harvested from these areas. This may be the result of prior surgery or simply because of the amount of tissue available in these areas, which varies from one person to the next. The buttock is an alternative donor site. A flap taken from this site, known as the gluteal artery perforator flap or “GAP flap,” can be used for breast reconstruction. As is the case with the DIEP flap, muscle is left in place at the GAP flap donor sites to preserve function and make recovery easier.
THE BUTTOCK AS A DONOR SITE
With GAP flaps, tissue for breast reconstruction can be harvested from either the upper or lower buttock, depending upon body shape and personal preference. The blood vessels needed for either an SGAP or IGAP flap are meticulously separated from the gluteus maximus muscles in which they travel without removing any muscle.
SGAP Flap (upper buttock):
The superior gluteal artery is employed when the upper buttock tissue is used for the reconstruction. Sometimes, it is possible to take tissue from the from the “love handle” area just above the buttock using a technique called LAP flap reconstruction. The shape of a women’s body will be an important factor in determining which procedure to perform.
IGAP Flap (lower buttock):
The IGAP flap is harvested from the lower buttock. The scar that results from harvest of this flap is designed to lie within the natural lower buttock crease. The IGAP flap is seldom used any more as it has generally been supplanted by the PAP flap.
MUSCLE-PRESERVING SURGERY
The blood vessels that are incorporated into an IGAP or SGAP flap are connected to blood vessels at the mastectomy site using microsurgical techniques. After the blood vessels of the flap are connected, a GAP flap is shaped into a new breast.
SGAP Breast Reconstruction in Connecticut and New York
Please Contact us if you would like more information about SGAP flaps, IGAP flaps, LAP flaps or PAP flaps for breast reconstruction, or for information about other options for breast reconstruction including DIEP flap surgery after mastectomy. Our practice has offices in New York City; in Fairfield County in Greenwich Connecticut; and on the campus of Vassar Brothers Medical Center, in the Hudson Valley.
One-Step Breast Reconstruction with Implants

One-Step Breast Reconstruction with Implants
Prepectoral Implant Reconstruction
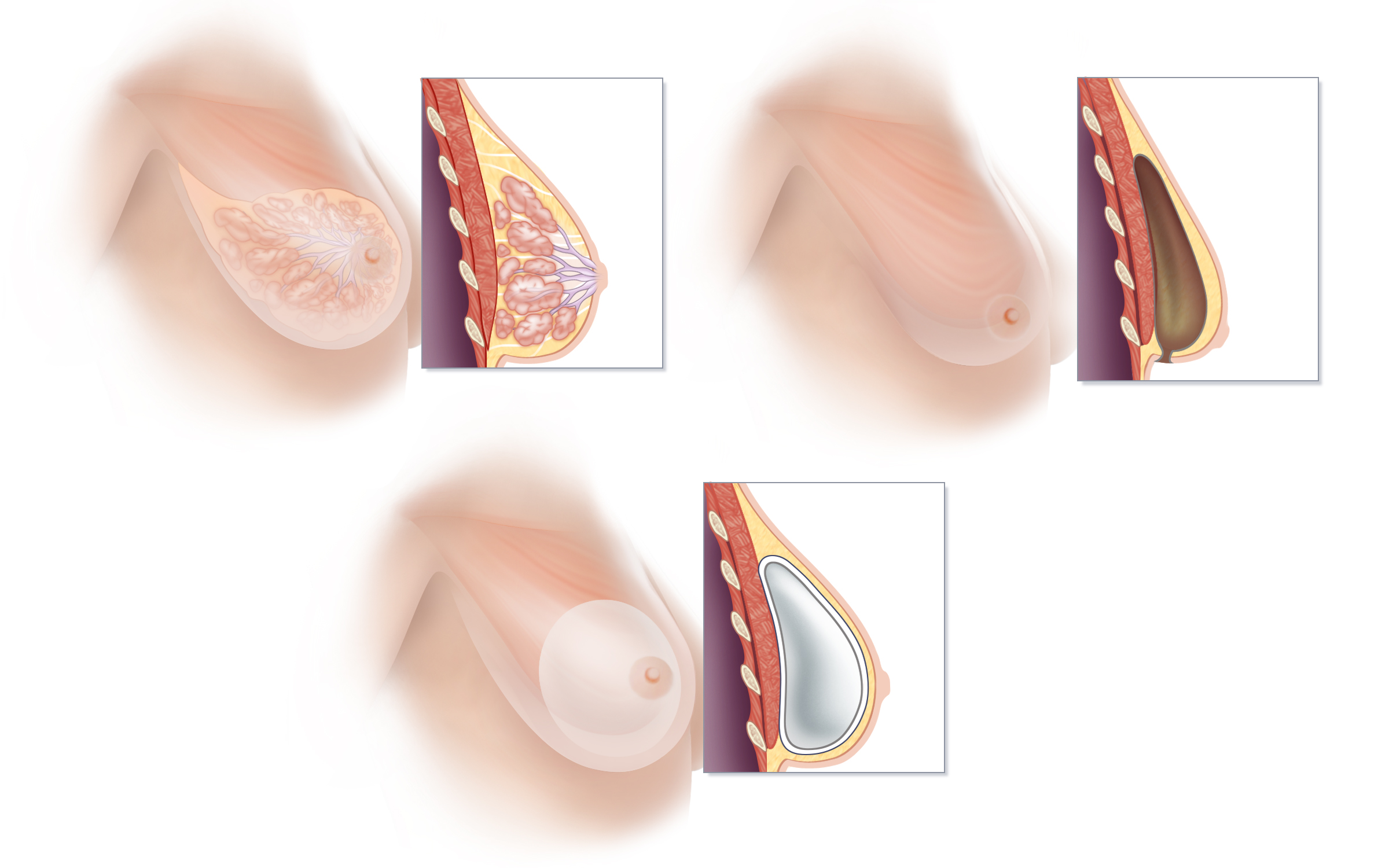
Prepectoral breast implant reconstruction is the current state-of-the-art method of implant-based breast reconstruction. This technique places an implant directly into the same space in which breast tissue is located prior to mastectomy. (A) Breast tissue is located on top of the muscles of the chest, between the pectoralis muscle and the skin. The lobules of the breast drain into a system of ducts that ultimately emerge through the nipple. (B) A mastectomy removes the tissue of the breast, and in so doing, inherently creates an empty space between the pectoralis muscle and the breast skin. (C) Prepectoral breast reconstruction restores the shape of the breast using an implant placed directly into the empty space created by mastectomy. Without disturbing the pectoralis muscle, a silicone-filled implant wrapped in specialized material known as acellular dermal matrix is inserted immediately following mastectomy. Prepectoral reconstruction avoids the weakness, discomfort, and visible movement of implants that can occur with muscle contraction (known as “animation deformity”) that commonly occur following traditional “under the muscle” implant (should this be implant-based) breast reconstruction.
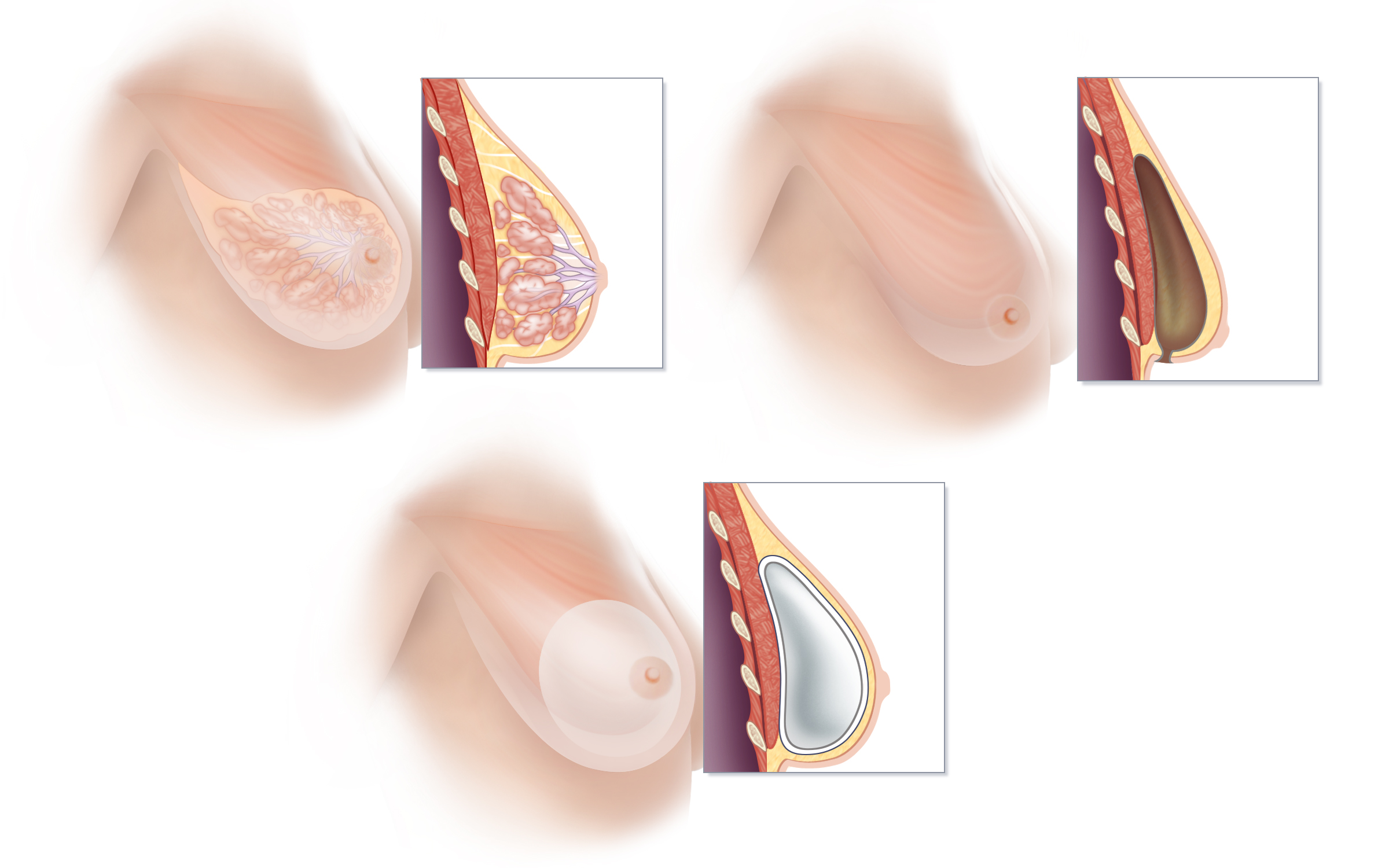
Prepectoral breast implant reconstruction is the current state-of-the-art method of implant-based breast reconstruction. This technique places an implant directly into the same space in which breast tissue is located prior to mastectomy. (A) Breast tissue is located on top of the muscles of the chest, between the pectoralis muscle and the skin. The lobules of the breast drain into a system of ducts that ultimately emerge through the nipple. (B) A mastectomy removes the tissue of the breast, and in so doing, inherently creates an empty space between the pectoralis muscle and the breast skin. (C) Prepectoral breast reconstruction restores the shape of the breast using an implant placed directly into the empty space created by mastectomy. Without disturbing the pectoralis muscle, a silicone-filled implant wrapped in specialized material known as acellular dermal matrix is inserted immediately following mastectomy. Prepectoral reconstruction avoids the weakness, discomfort, and visible movement of implants that can occur with muscle contraction (known as “animation deformity”) that commonly occur following traditional “under the muscle” implant (should this be implant-based) breast reconstruction.
When used for breast reconstruction, breast implants can be placed on top of the pectoralis major muscle, using a technique called “pre-pectoral breast reconstruction” or under the pectoralis major muscle using the traditional “submuscular” approach.
Traditionally, women who have undergone implant reconstruction following mastectomy have initially had a tissue expander placed under the pectoralis chest muscle. Following an expansion process that requires regular visits to the surgeon’s office (in order to stretch the pectoralis muscle and create ample room for a breast implant of the desired size), a second surgery is done to remove the tissue expander and exchange it for a breast implant.
Our surgeons are part of group of innovative plastic surgeons who challenge the idea that implants must always be placed under the pectoralis muscle. To us, it simply makes the most sense, whenever possible, to replace volume directly where it is missing—right in the space that is left following mastectomy—rather than disrupt important and sizeable muscles, such as the pectoralis major muscle. This approach is favored in many cases because it is the philosophy of our team, regardless of the type of reconstruction we are performing, to preserve as much of a woman’s natural anatomy as possible, and to minimize interference with muscle function, strength and motion.
In comparison to techniques that place an implant under the pectoralis muscle, the placement of an implant in front of the pectoralis muscle means less pain, quicker recovery, less chronic discomfort or fatigue and less disruption of function. Furthermore, implants placed on top of the muscle do not flex or become distorted with pectoralis muscle flexion, upper body movements or exercise. Therefore, the unnatural movement and distortion of implants that is commonly seen when “under-the-muscle” implant reconstruction patients are moving their upper bodies or exercising (known as “muscle flex deformity” or “dynamic distortion”) is avoided. In fact, we sometimes relocate implants from below to above the muscle for women who are troubled by muscle-flex deformities.
Pre-pectoral implant reconstruction and traditional “behind the muscle” implant reconstructions each have certain advantages and disadvantages, so selecting which approach to recommend is done on a case by case basis.
The type of reconstruction you ultimately select should take into account the cancer treatment you require, your body type, your lifestyle, and your own goals for reconstruction. The risks and benefits of each type of breast reconstruction will be explored in detail at the time of your consultation.
Body Lift Breast Reconstruction with “Extended DIEP Flaps”

Body Lift Breast Reconstruction with “Extended DIEP Flaps”
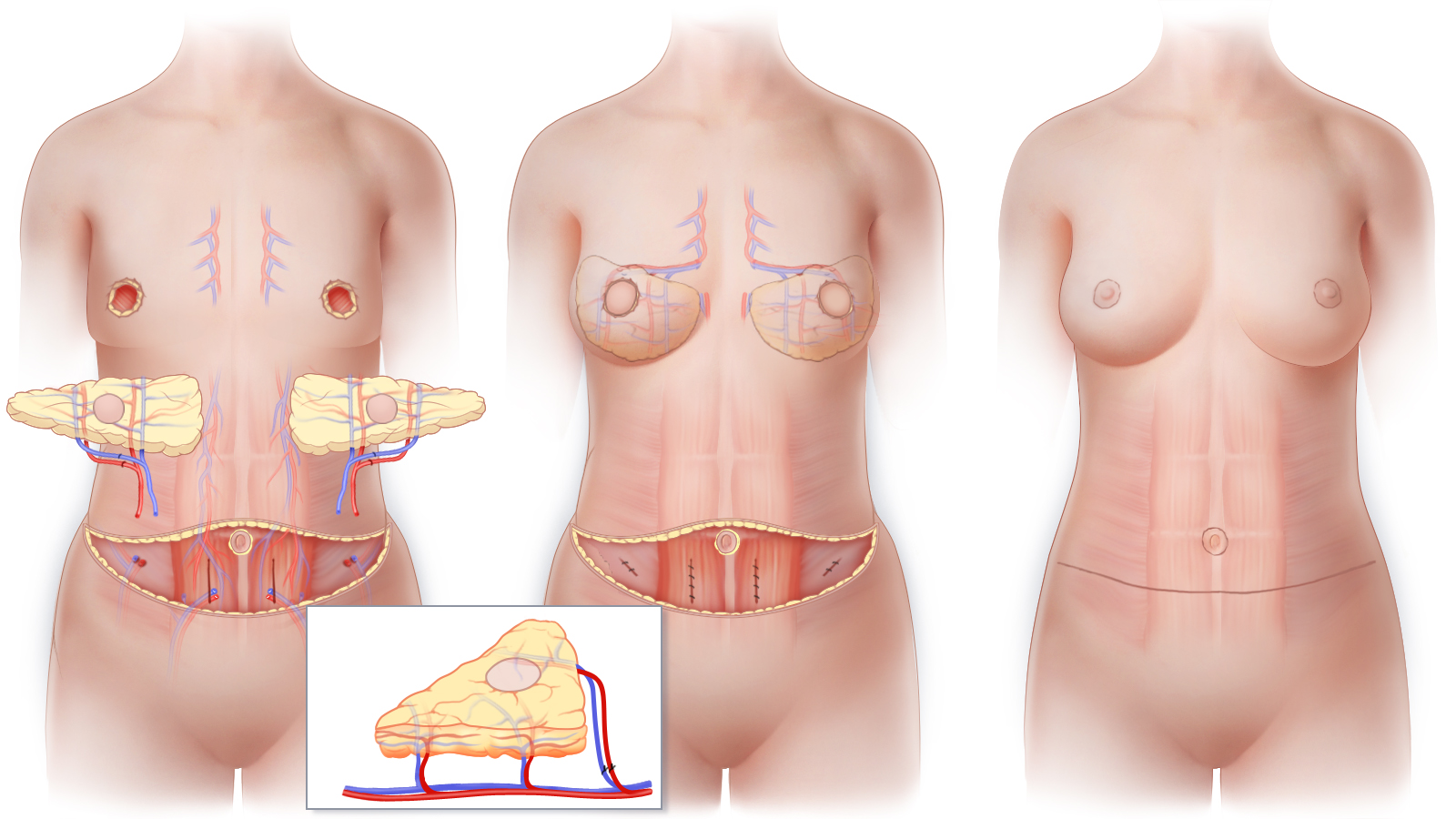
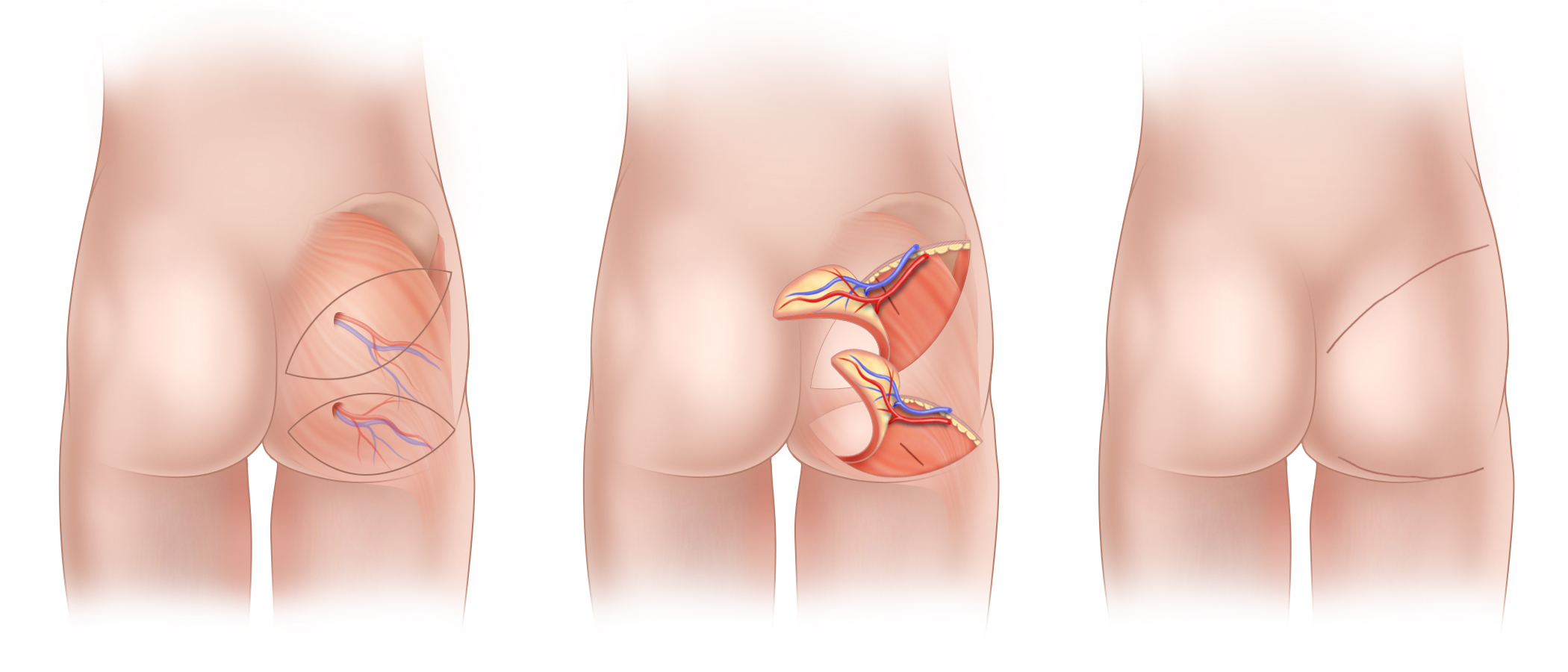
“Body Lift Breast Reconstruction” uses four flaps in total to reconstruct two breasts. With this approach, it is possible to reconstruct both breasts and achieve a larger breast size than could be achieved with a single DIEP flap for each breast. Body Lift Breast Reconstruction uses a DIEP flap from each side of the abdomen in combination with a second flap prepared from the tissue of the flank or “love handle” area. (A) The blood vessels that supply each of the four individual flaps used in this technique are meticulously separated from muscle, thus leaving muscle intact and functioning. (Inset) The blood vessels of two individual flaps are shown interconnected to one another in preparation for transfer to the chest. This procedure is performed on both sides of the abdomen to create two sets of stacked flaps. (B) The two sets of stacked flaps are transferred to the chest and, using microsurgical techniques, connected to blood vessels that will nourish the newly reconstructed breasts. (C) As is the case with body lift surgery, Body Lift Breast Reconstruction sculpts the waistline, flanks, and in some cases, outer thighs.
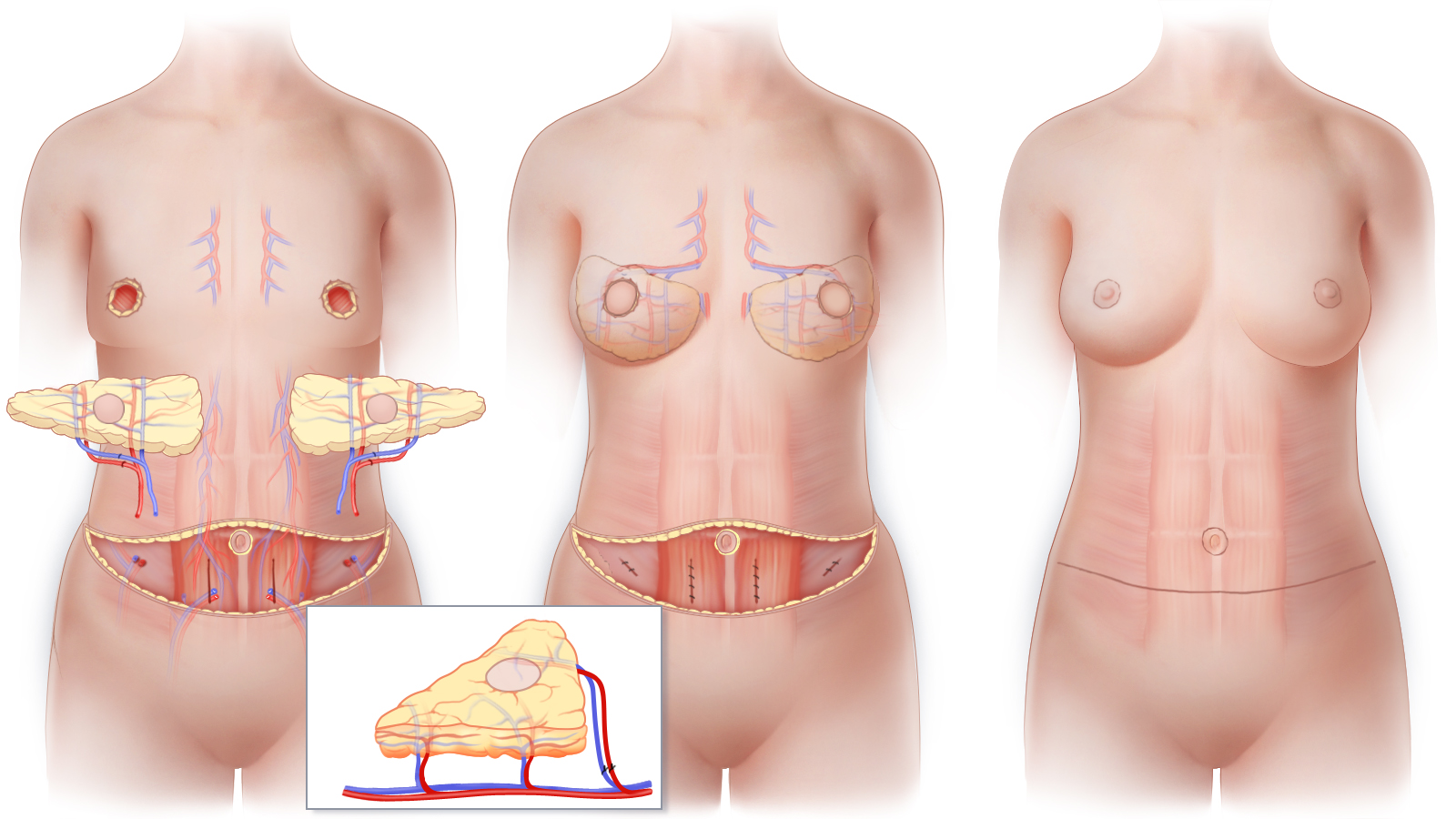
“Body Lift Breast Reconstruction” uses four flaps in total to reconstruct two breasts. With this approach, it is possible to reconstruct both breasts and achieve a larger breast size than could be achieved with a single DIEP flap for each breast. Body Lift Breast Reconstruction uses a DIEP flap from each side of the abdomen in combination with a second flap prepared from the tissue of the flank or “love handle” area. (A) The blood vessels that supply each of the four individual flaps used in this technique are meticulously separated from muscle, thus leaving muscle intact and functioning. (Inset) The blood vessels of two individual flaps are shown interconnected to one another in preparation for transfer to the chest. This procedure is performed on both sides of the abdomen to create two sets of stacked flaps. (B) The two sets of stacked flaps are transferred to the chest and, using microsurgical techniques, connected to blood vessels that will nourish the newly reconstructed breasts. (C) As is the case with body lift surgery, Body Lift Breast Reconstruction sculpts the waistline, flanks, and in some cases, outer thighs.
For women whose tummy tissue is not adequate or sufficient enough for ordinary DIEP flap reconstruction, “Body Lift Breast Reconstruction,” or “extended DIEP” flap breast reconstruction, can be a solution for restoring both breasts with natural living tissue. Just as stacked DIEP flaps can provide the necessary tissue to restore one breast when a single DIEP flap is not enough, Body Lift Breast Reconstruction is an option when one DIEP flap for each breast is just not enough. Using two flaps for each breast—four flaps in total—with the flaps folded, layered or “stacked” upon each other, gives added size and projection to the new breasts, especially for women who would not have enough tissue to be a candidate for traditional DIEP flap reconstruction, and/or have been told that they “do not have enough tissue” for a natural-tissue breast reconstruction.
Double-stacked breast reconstruction is most commonly done using a “body lift” technique. We design the perforator flaps used in this surgery much the same way that cosmetic plastic surgeons design a body lift. By combining DIEP flaps from the front of the abdomen with perforator flaps taken from the flank or “love handle” area (typically Deep Circumflex Iliac Artery or DCIA flaps), the extended DIEP flap technique reshapes the tummy and waist to produce an hourglass silhouette. Less frequently, we combine DIEP flaps from the abdomen with flaps taken from the thighs, in what is sometimes called a “four-flap” breast reconstruction. Regardless of which approach we use, our goal is to maximize the aesthetic results at the breasts as well as at the site of the “donated” tissue.
Muscle Preserving surgery
Blood vessels that are used for “Body Lift Breast Reconstruction” or “Four Flap Breast Reconstruction” are meticulously dissected without removing or destroying muscle. Because muscle is preserved, postoperative pain and discomfort are minimized, and strength and function are preserved. After the tissue that will form each new breast is transferred to the chest, the blood vessels that will nourish each flap are connected to blood vessels at the mastectomy site using delicate microsurgical techniques. When possible, sensory nerves may be connected to facilitate recovery of sensation in a reconstructed breast. Finally, the tissue is shaped into a new breast.
Abdominal Contouring
Because the lower abdominal tissue used for “Body Lift Breast Reconstruction” or “Four Flap Breast Reconstruction,” is similar to that removed during a tummy-tuck, or body-lift cosmetic procedure, women who undergo this procedure generally benefit from an improvement in the contour of their abdomen and waist. While typically not as low as the scar of a tummy-tuck, the scar that results from this type of surgery can typically be concealed in most clothing and in a once-piece bathing suit.
Optimizing Aesthetics
Approximately three months after the initial stage of breast reconstruction surgery, refinement of breast shape and procedures to produce overall symmetry can be completed. These optional additional procedures are performed on an outpatient basis and are referred to as Stage II.
Body Lift Breast Reconstruction IN CONNECTICUT and NEW YORK
Contact us if you would like more information about body lift breast reconstruction or for information about other options for breast reconstruction including DIEP flap surgery after mastectomy or breast reconstruction using breast implants. Our practice has offices in New York and Fairfield County, Greenwich Connecticut, and on the campus of Vassar Brothers Medical Center, in the Hudson Valley.
Reconstruction with Tissue Expanders and Implants

Reconstruction with Tissue Expanders and Implants
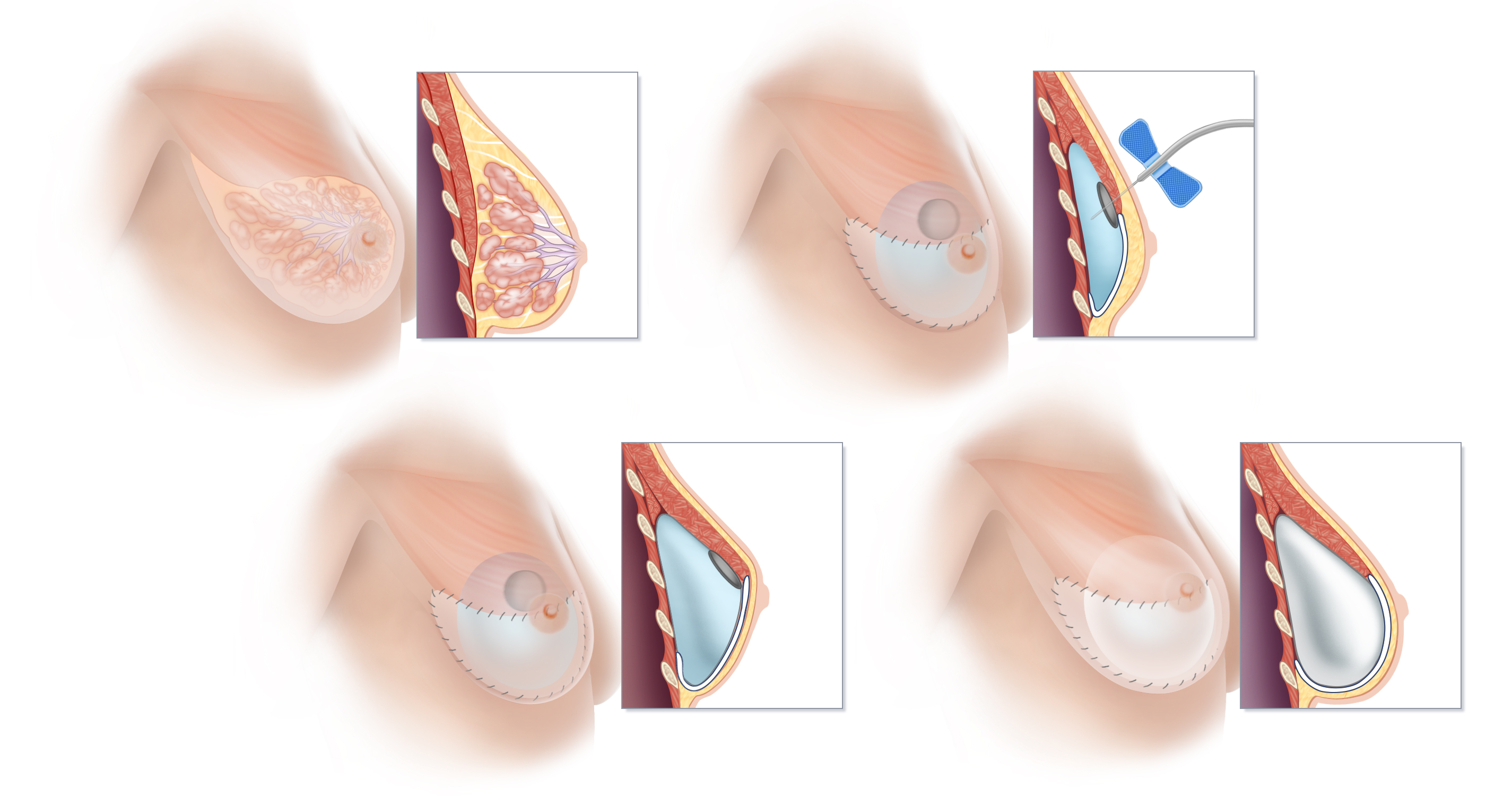
(A) Breast tissue is located on top of the muscles of the chest, between the pectoralis muscle and the skin. The lobules of the breast responsible for milk production drain into a system of ducts that travel to the nipple. If a woman’s reconstructive plan calls a breast implant to be placed “under the muscle,” the pectoralis muscle must be stretched out to create ample space for the implant. In order to create this space, the lower edge of the pectoralis major is surgically separated from the chest wall, and a tissue expander is inserted beneath this muscle. The lower portion of the tissue expander is then typically covered with a specialized acellular dermal matrix to provided added support. (B) At each of a series of office visits following recovery from surgery, the tissue expander is gradually inflated by injection with sterile fluid or air. (C) Once the tissue expander is fully expanded and sufficient space created, an additional surgical procedure is scheduled to remove the expander and replace it with a breast implant. (D) Below the stretched-out pectoralis muscle, a breast implant has replaced the tissue expander. In many cases, the stretched muscle will cover only the upper portion of the implant, and more complete coverage of the breast implant is accomplished by using a tissue matrix such as AlloDerm or Dermacell® between the lower edge of the pectoralis muscle and the chest wall.
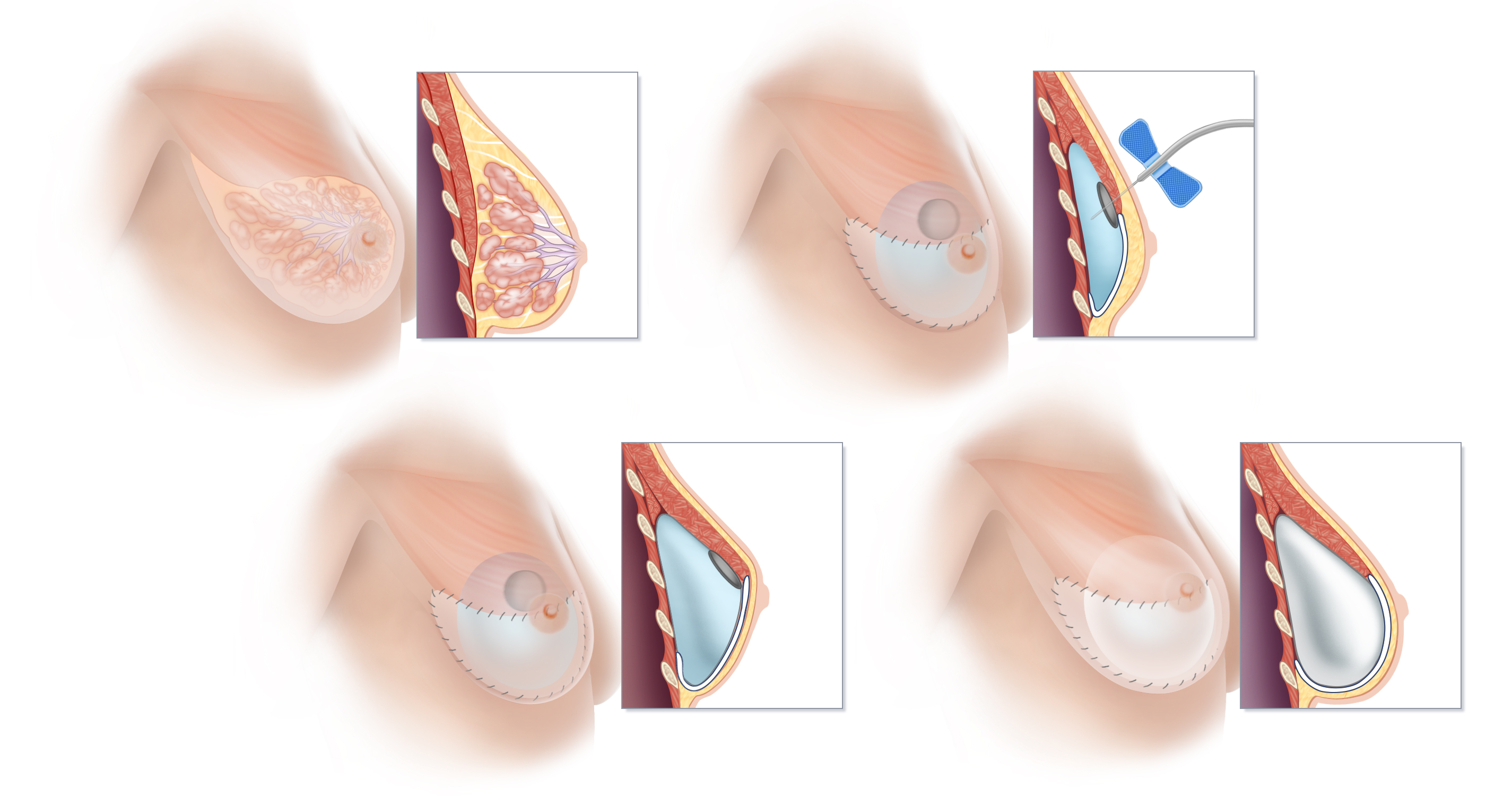
(A) Breast tissue is located on top of the muscles of the chest, between the pectoralis muscle and the skin. The lobules of the breast responsible for milk production drain into a system of ducts that travel to the nipple. If a woman’s reconstructive plan calls a breast implant to be placed “under the muscle,” the pectoralis muscle must be stretched out to create ample space for the implant. In order to create this space, the lower edge of the pectoralis major is surgically separated from the chest wall, and a tissue expander is inserted beneath this muscle. The lower portion of the tissue expander is then typically covered with a specialized acellular dermal matrix to provided added support. (B) At each of a series of office visits following recovery from surgery, the tissue expander is gradually inflated by injection with sterile fluid or air. (C) Once the tissue expander is fully expanded and sufficient space created, an additional surgical procedure is scheduled to remove the expander and replace it with a breast implant. (D) Below the stretched-out pectoralis muscle, a breast implant has replaced the tissue expander. In many cases, the stretched muscle will cover only the upper portion of the implant, and more complete coverage of the breast implant is accomplished by using a tissue matrix such as AlloDerm or Dermacell® between the lower edge of the pectoralis muscle and the chest wall.
Breast implants used in breast reconstruction can be placed either on top of the pectoralis major muscle, using a technique called “pre-pectoral breast reconstruction” or under the pectoralis major muscle using the traditional “submuscular” approach.
Because the goal of practice is to try to preserve a woman’s natural anatomy as much as possible and avoid interfering with muscle function, strength and comfort, when possible we generally favor placing implants on top of the muscle. However, for a variety of reasons, reconstruction using the pre-pectoral implant technique may not be possible.
If for any reason an implant cannot be placed on top of the pectoralis muscle in the space created by mastectomy, a tissue expander can be used to prepare for breast implant reconstruction. Similarly, if a woman decides to have a breast reconstructed with an implant at some later time––after undergoing mastectomy without reconstruction–– tissue expansion will generally be required. By contrast, a tissue expander is almost never required for women who choose natural-tissue breast reconstruction, even if some time has elapsed since the mastectomy.
A tissue expander is a temporary inflatable implant designed to stretch the skin and muscle of the chest in order to make room for a more permanent implant. Tissue expanders used in breast reconstruction are generally placed below the pectoralis muscle. An expander is like an adjustable balloon that can be inflated gradually over a period of a few months to make enough room to later accommodate an implant behind the stretched-out muscle and skin.
Women who undergo expander/implant reconstructions typically visit the office every few weeks after surgery to have the expander filled by injecting it with sterile fluid. This process can be somewhat uncomfortable, and may cause you to feel stiff or tight in the area. Once ample expansion is achieved, a second surgery will be done to remove the tissue expander and replace it with the breast implant.
Learn more about the lifespan of implants and about natural-tissue breast reconstruction as an alternative to breast implants.
The type of reconstruction you ultimately select should take into account the cancer treatment you require, your body type, your lifestyle, and your own goals for reconstruction. The risks and benefits of each type of breast reconstruction will be explored in detail with you at the time of your consultation.
Implant Breast Reconstruction in New York and Connecticut
Contact us to schedule a consultation, or if you would like more information about the options for breast reconstruction after mastectomy. Our practice has offices in Greenwich, Connecticut and New York. We perform breast reconstruction surgery at several hospitals in Connecticut and New York.
Patient Letters

Medical Articles

Breast Cancer and Reconstruction News

For Clinicians

Am I A Candidate?

Breast Cancer

Breast Cancer
What Is Breast Cancer?
Breast cancer occurs when cells of the breast grow in an unrestrained or abnormal manner, increasing both in size and in number. Cancer cells can interfere with the normal function of the breast and can also spread to other parts of the body.
Breast Cancer Statistics
With the exception of skin cancer, breast cancer is the most common cancer among American women; about one in eight will have a diagnosis of breast cancer. Every year, more than 210,000 women will be diagnosed according to the National Institutes of Health and the American Cancer Society. Carcinoma in-situ, the earliest form of breast cancer (sometime called “pre-cancer”) will affect nearly 60,000 additional women in the United States each year.
There is some good news, however. Recent data show:
- A decrease in the number of new breast cancer diagnoses
- Improved survival for those women who have breast cancer.
There are presently about 2.5 million breast cancer survivors in the United States. Improved survival is likely the result both of early diagnosis and of advances in available treatment.
Breast Cancer and Breast Reconstruction
Almost every women who will, or has already undergone a mastectomy is potentially a candidate for breast reconstruction surgery. In fact, a number of states, including New York State, have recently enacted laws that require hospitals to inform breast cancer patients about breast reconstruction options. Each method of reconstruction has its own benefits and risks and not every method will appeal to every woman (if any appeal at all). Understanding the options for breast reconstruction can help you feel more secure as you make important decisions about the kind of care and treatment that will be best for you.
Patients Supporting Patients

Patients Supporting Patients
You may find it helpful to connect with someone who has had similar experiences when you’re making decisions about breast cancer care and breast reconstruction. Several of our patients have generously volunteered to be part of a support network for women considering breast reconstruction surgery.
If you would like to be put in touch with one of these volunteers, either by phone or by email, please let our office know, and we will arrange for you to be in touch with some of our Patients Supporting Patients volunteers.
Our Offices
- New York Office
- 1776 Broadway
Suite 1200
New York, NY 10019
212 744-1200
- Connecticut Office
- 77 Lafayette Place
Suite 302
Greenwich, CT 06830
203 863-0003
Resources

Breast Reconstruction and Cancer Resources
Patients Supporting Patients
You may find it helpful to connect with someone who has had similar experiences when you’re making decisions about breast cancer care and reconstruction. If you would like to talk with one of our patients who have volunteered to be part of a support network for women considering breast reconstruction surgery, please let us know.
Breast Reconstruction Medical Articles
Dr. Greenspun has written numerous articles that have been published in peer-reviewed medical and scientific journals. Links to selected publications are provided.
Myths About DIEP Flaps
Misunderstandings and misconceptions about perforator flap surgery abound. Perhaps because so few plastic surgeons perform these procedures on a regular basis, obtaining accurate and reliable information can at times be difficult. We attempt to clarify a number of the more common myths in this section.
Your Legal Rights
Both Federal and State Laws protect a woman’s right to obtain insurance coverage for breast reconstruction surgery. In addition, Federal law also provides protection against discrimination by health insurance companies and employers on the basis of a person’s genetic makeup
For Clinicians
Healthcare providers can make referrals electronically. In addition, access to recent publications about breast reconstruction are available.
Am I a Candidate?
By answering just a few questions we can help you find out if you are a candidate for reconstructive breast surgery.
Frequently Asked Questions
Find answers to frequently asked questions about perforator flap microsurgical breast reconstruction.
Breast Cancer & Reconstruction Links
Links to external websites that provide information or resources that may be of interest to people seeking information about topics such breast cancer, breast reconstruction, and the BRCA gene are provided.
Procedures & Techniques

State-of-the-Art Approaches to Breast Reconstruction
Broadly speaking, breast reconstruction procedures fall into one of two categories:
- Breast reconstruction using natural tissue from your own body
- Breast reconstruction using breast implants
Natural tissue generally provides the most natural-appearing (and feeling), as well as most durable type of breast restoration. Some women, however, may prefer reconstruction with breast implants, especially if they want to avoid a scar on a location other than the breast/s.
Natural Tissue
Living tissue that is surgically relocated from one part of the body to another is called a “flap.” The most advanced methods of natural-tissue breast reconstruction, known collectively as perforator flaps, use natural tissue to restore a breast without compromising a woman’s muscles in the process. These procedures can be performed with a minimal amount of pain. They typically result in a reconstructed breast that is warm, soft and forever part of a woman’s body. Our practice has roughly a 99.5% success rate for these procedures. Because perforator flaps do not remove muscle, these procedures are now considered by many experts to be the gold standard for natural-tissue breast reconstruction.
Click here to learn about specific options for natural tissue breast reconstruction surgery
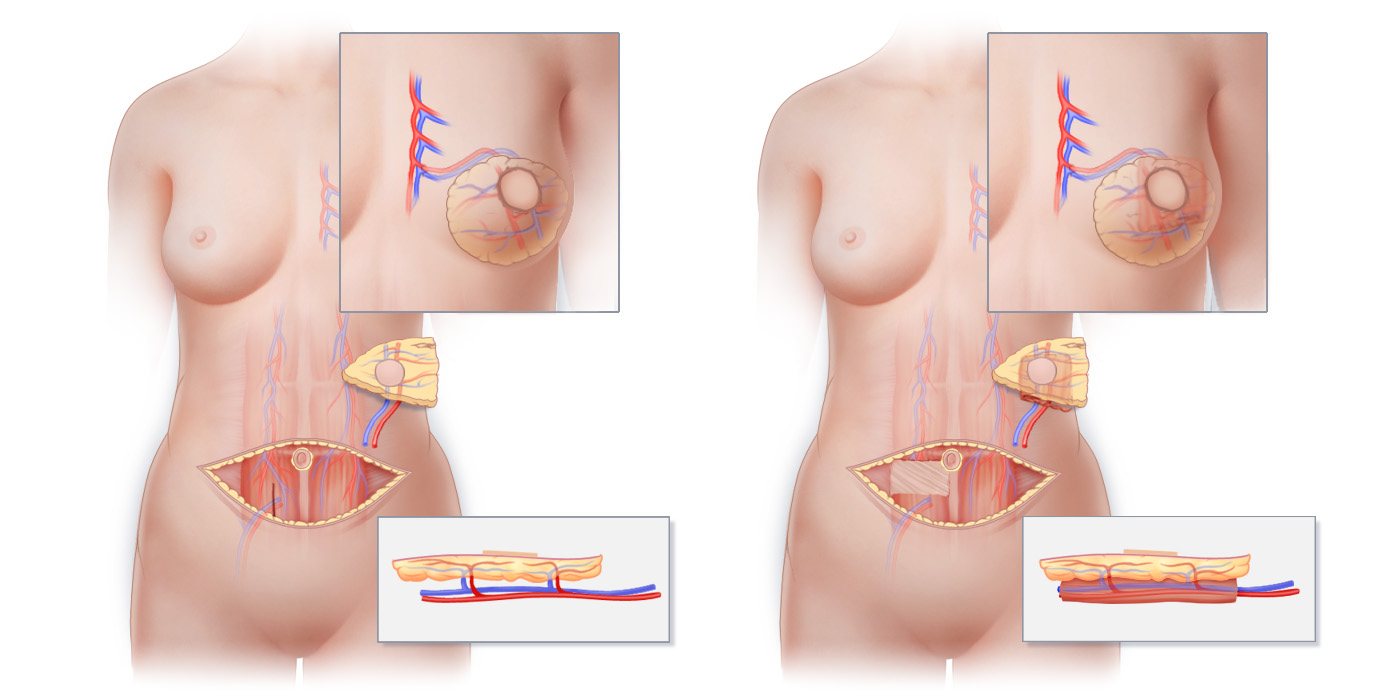
Breast Implants
For women who opt to have breast reconstruction using breast implants, it is now sometimes possible to place a breast implant directly into the space created by the mastectomy, just underneath the skin of the breast. This approach, sometimes called pre-pectoral breast implant reconstruction, is currently the most state-of-the-art approach to reconstruction using breast implants. While not suitable in every situation, it is often preferred over the traditional approach of tissue expander/breast implant reconstruction that involves surgical disruption of the muscles of the chest that can be painful in the short term, and may compromise muscle function and be uncomfortable in the long term.
Click here to learn about specific options for breast reconstruction using breast implants
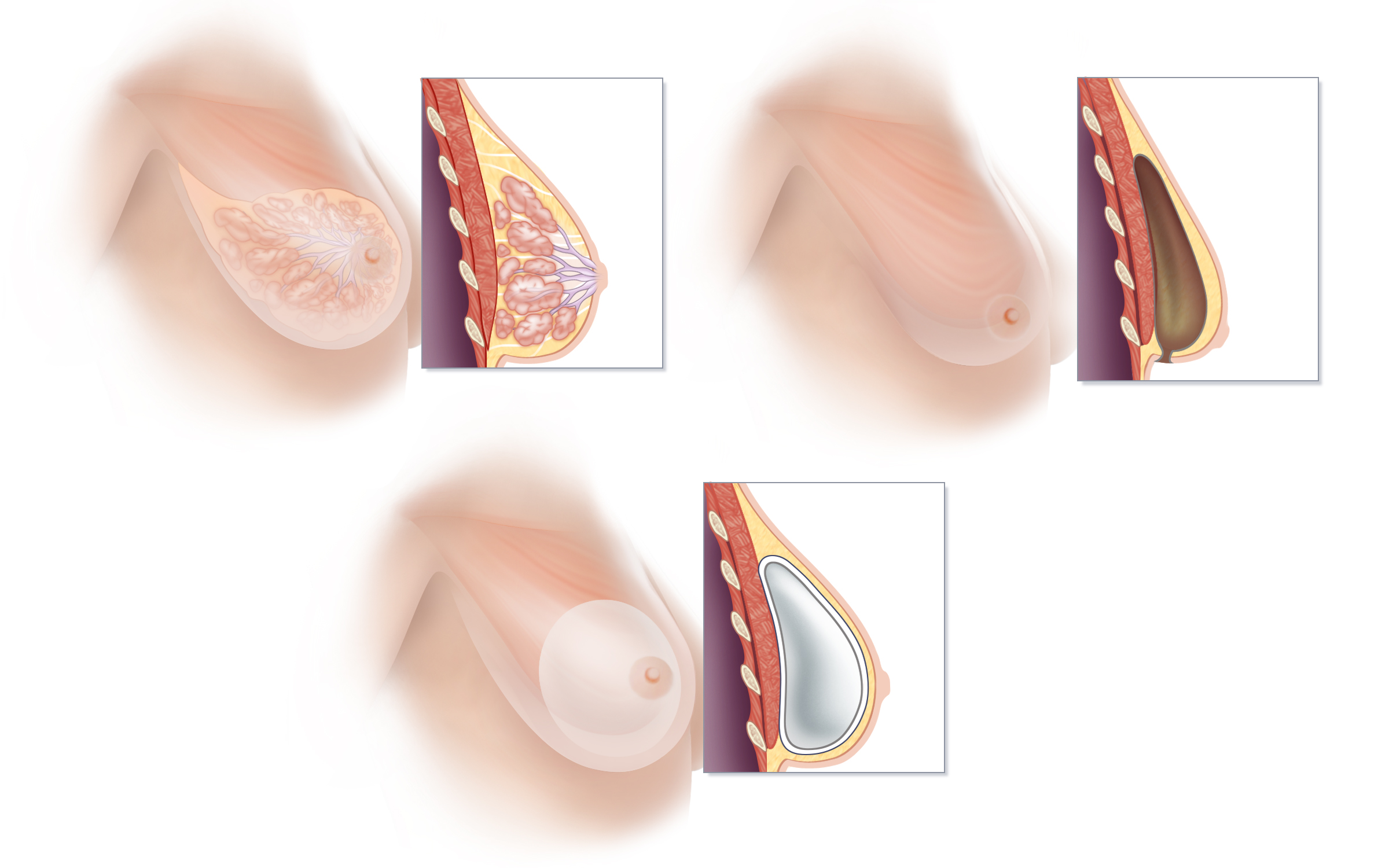
Radiation & Reconstruction

Radiation & Breast Reconstruction
The Effects of Radiation on Breast Reconstruction
When radiation is used in the treatment of breast cancer, non-cancerous tissues in the path of the radiation are also affected. Radiation therapy can mean a significant loss of skin elasticity, which can profoundly affect the aesthetic results of breast reconstruction. And because the body’s wound-healing mechanisms are altered by exposure to radiation, complications from all types of reconstructive breast surgery occur at a higher rate.
Radiation is especially problematic for women who undergo implant reconstructions, regardless of whether the radiation is administered before or after the implant is placed. Natural-tissue reconstruction has the benefit of bringing non-radiated, healthy, well-vascularized tissue to the mastectomy site, and this can actually aid in the healing process.
Because of the potential complications associated with implants, breast reconstruction using natural tissue is generally considered the best method for women who will require or have already had radiation.
While radiation therapy can complicate breast reconstruction surgery, with proper preparation most women can achieve a satisfactory reconstruction even if radiation therapy is part of their treatment plan. Perforator flaps including the DIEP flap, SIEA flap and SGAP flap are all used routinely with excellent results to reconstruct patients who have required radiation therapy.
Timing of Reconstructive Surgery When Radiation Therapy is Necessary
The need for radiation may, however, be a factor in determining if a woman will undergo an immediate or a delayed breast reconstruction; radiation may also influence which method of reconstruction she chooses.
Ideally, to achieve the best cosmetic results and minimize the chances of complications, we prefer to wait approximately six months before performing a perforator flap reconstruction when a woman has had radiation therapy. This time period may vary, depending on each woman’s particular circumstances. By waiting, we can replace radiation-damaged skin with soft and supple skin that has not been exposed to any radiation. Doing so allows for the shaping of a more natural-appearing breast and also reduces the chance of complications. Nevertheless, in certain circumstances, reconstruction can still be done ahead of radiation.
The need for radiation therapy cannot always be determined prior to mastectomy surgery. And on occasion, a woman may already have begun the reconstructive process after mastectomy when she learns that she will need to undergo radiation treatment. Since treatment of the cancer takes precedence, radiation will take place whenever the oncologist thinks it best, and our practice will take all appropriate measures to manage any complications that may arise and to optimize the final reconstruction.
» Contact us if you would like to make an appointment and learn more about your options
Tubular Breasts

TUBULAR BREASTS
One of the most common abnormalities of breast shape is called a tubular breast. Such breasts, also known as tuberous breasts or constricted breasts, result from congenital variation in the development of the breast tissue that can affect one or both breasts. Although there is considerable variation, tubular breasts all share some common features.
Tubular breasts are characterized by:
- Narrow and elongated shape
- Little or no breast tissue in the lower half of the breast
- An areola (pigmented area around the nipple) that appears disproportionately large
- Protrusion of the breast tissue behind the nipple and areola that makes the nipple and areola look puffy
- A wide space between the breasts
- Tendency for the location at which the underside of the breast joins the chest (known as the inframammary fold) to be relatively high on the chest, thus causing the breast to droop and look long and constricted.
Surgical Correction
Surgery to correct tubular breasts is challenging. The most commonly performed procedures almost always augment the breast, either with an implant or using a woman’s own tissue. In addition to adding volume to the breast, the base of the breast must be widened to a normal size, the inframammary fold lowered and the internal constrictions that caused the tubular shape must be released with internal incisions. In addition, the areola is usually reduced in size.
Breast implants have traditionally been used to provide the volume needed to correct a tuberous breast. Although implants continue to be widely used, both perforator flaps and fat grafting can be used as alternatives to breast implants. In particular, the DIEP flap and the TDAP flap have been effective in correcting tubular breast deformity. By using your own tissue, complications unique to breast implants (implant leakage or rupture, rippling, and capsular contracture) can be avoided. Reconstruction using your own tissue means a having a reconstruction with tissue that is yours for life and without having to worry about needing to replace implants from time to time.. Since there is a great deal variability in the severity of tubular breast deformities, the approach or approaches best suited to you will depend upon the condition of your breasts and your goals for reshaping them. Depending both on the severity of the condition and on your insurance benefits, coverage for surgery to correct tubular breasts may be available.
» Learn more about sophisticated natural-tissue alternatives to breast implant reconstruction
» Contact us if you would like to make an appointment and learn more about your options
BRCA1 & BRCA2

BRCA1, BRCA2 and BRACAnalysis® Testing:
The BRCA genes function to keep breast cells growing normally and to prevent cancer-cell growth. Scientists have identified mutations of the BRCA1 and BRCA2 gene that can make someone susceptible to developing breast and/or ovarian cancer at some point in their life. When these genes contain the mutations, they do not function normally, and cancer risk increases. Mutations in these genes can be passed from either parent to their children.
- The lifetime risk of developing breast cancer is as high as 84% for women who have inherited a BRCA1 or BRCA2 mutation.
- The lifetime risk of developing ovarian cancer is as high as 60% for women who carry a BRCA1 or BRCA2 genetic mutation.
A blood test, or a cheek swab test called BRCAnalysis®, can determine if someone carries a BRCA1 or BRCA2 gene mutation and empower him or her to make informed choices about risk reduction surgery such as prophylactic mastectomy. Our office can help arrange for this testing for women at risk.
Women who have a strong family history of breast cancer but who do not carry the BRCA1 or BRCA2 gene mutations should keep in mind that a significant proportion of all hereditary breast cancer may be caused by mutations in genes other than BRCA1 and BRCA2. In other words, if you are “BRCA negative” but have strong family history of breast cancer, you may have inherited a different gene (for which a test to identify it does not exist) that puts you at higher than average risk for developing breast cancer.
Please c ontact us if you would like to make an appointment and learn more about BRCA gene testing, your options for risk-reducing prophylactic mastectomy or reconstruction with perforator flaps such as the DIEP flap.
Poland’s Syndrome

POLAND’S SYNDROME
This syndrome, named after Sir Alfred Poland, is characterized by variable underdevelopment of the breast, nipple, chest muscles, ribs and upper extremity on the side of the body affected by this condition. Both men and women can be affected. In milder cases, one breast does not develop fully during puberty, and as a result, is generally smaller than the uninvolved breast and may not have a conventional shape. Males with mild cases may simply notice that their chest appears to be slightly concave on the involved side. In more severe cases, the breast, nipple/areola and even the pectoralis muscle may be completely absent. Women with mild cases may notice that the involved breast is significantly smaller than the other side; in more severe cases, the breast may be completely abscent. In the most severe cases, the skeletal structure of the chest (ribs and breastbone) and the arm may also be affected. Except in the most severe cases, most people do not have any functional disability from Poland’s Syndrome.
Classic Methods of Correcting Breast and Chest Abnormalities
In order to correct these abnormalities in the appearance of the breast and chest, reconstructive surgery is commonly sought by both women and men affected by Poland’s Syndrome Female teenagers, typically, feel self-conscious, and may even experience intense anxiety as a result of abnormal or markedly assymetrical breast development. The type of surgery and the timing of such reconstructive surgery will depend on a number of factors including the person’s age and the severity of his or her condition.
Many different techniques have been used to correct these chest and breast abnormalities. Historically, tissue expanders, implants with or without latissimis dorsi muscle flaps, and TRAM muscle flaps are most commonly used to treat females with Poland’s Syndrome. Men have traditionally been treated with custom-fabricated implants and latissimis dorsi muscle flaps. While implant reconstruction is commonly suggested as a first step, the shortage of skin, breast tissue and sometimes muscle available to cover an implant makes achieving a satisfactory outcome with these procedures especially challenging.
Latest Surgical Options for Poland’s Syndrome
Newer methods of reconstruction now offer people with Poland’s Syndrome the option of undergoing reconstruction of the breast and chest using their own tissue but without having to sacrifice important functional muscles like the latissimis dorsi or the rectus abdominis for a TRAM flap. Breast reconstruction using a perforator flap such as the DIEP flap, SIEA flap, or TDAP flap can help restore the contour of the chest and breast without the use of an implant or muscle. Autologous fat grafting may also be an option for both men and women who have only mild cases of Poland’s Syndrome. These reconstructive procedures may be an attractive option when an implant is not desired or when an implant has previously been ineffective.
» Learn more about sophisticated natural-tissue alternatives to breast implant reconstruction
» Contact us if you would like to make an appointment and learn more about your options
Stacked DIEP Flap

Stacked DIEP Flap
Stacked Deep Inferior Epigastric Perforator Flap
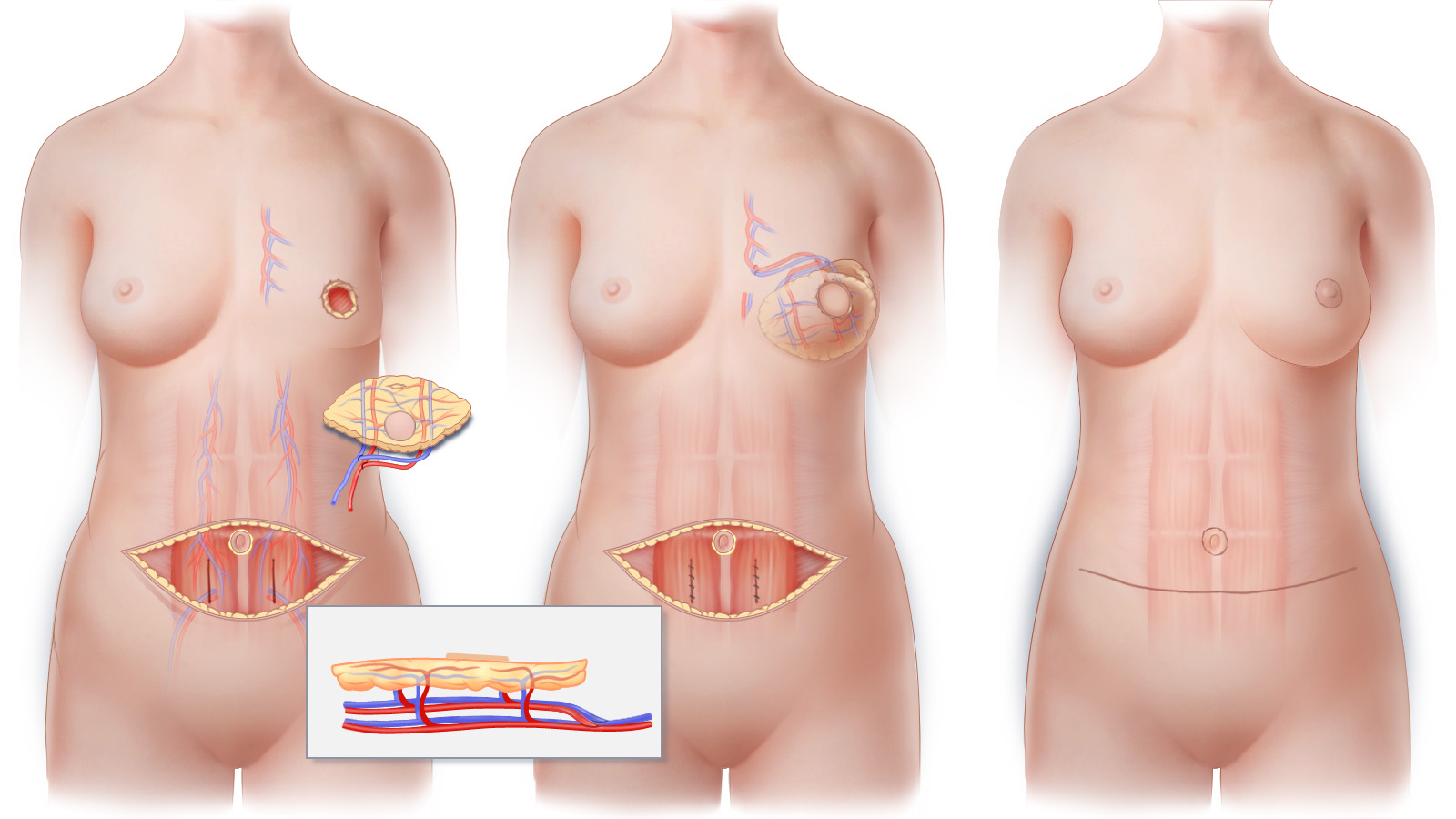
With a stacked-DIEP flap procedure, two DIEP flaps—one DIEP flap from each side of the abdomen— are used to reconstruct a breast of a larger size than could be reconstructed with just one DIEP flap. (A) The blood vessels that supply each individual DIEP flap are meticulously separated from the abdominal muscle, leaving the muscle intact. (Inset) Cross sectional view of stacked DIEP flaps showing the blood vessels of each individual flap interconnected to one another in preparation for transfer to the chest. (B) The stacked-DIEP flap is transferred to the chest and, using microsurgical techniques, connected to blood vessels at the recipient site that will nourish both DIEP flaps. (C) The horizontal abdominal scar that results following stacked-DIEP flap surgery is similar to that created by a “tummy tuck.” The scar that results on the breast will depend upon the technique used for mastectomy.
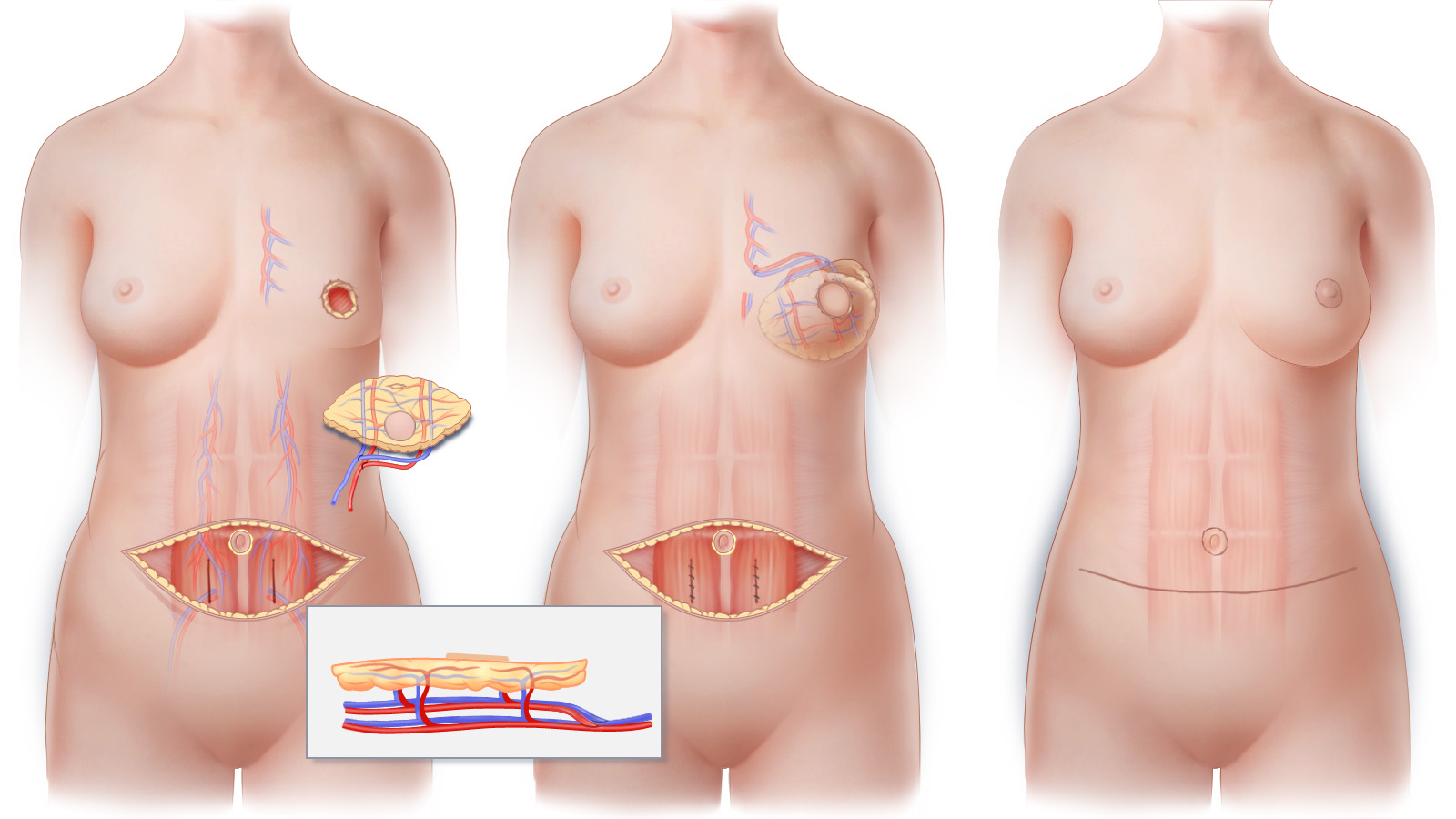
With a stacked-DIEP flap procedure, two DIEP flaps—one DIEP flap from each side of the abdomen— are used to reconstruct a breast of a larger size than could be reconstructed with just one DIEP flap. (A) The blood vessels that supply each individual DIEP flap are meticulously separated from the abdominal muscle, leaving the muscle intact. (Inset) Cross sectional view of stacked DIEP flaps showing the blood vessels of each individual flap interconnected to one another in preparation for transfer to the chest. (B) The stacked-DIEP flap is transferred to the chest and, using microsurgical techniques, connected to blood vessels at the recipient site that will nourish both DIEP flaps. (C) The horizontal abdominal scar that results following stacked-DIEP flap surgery is similar to that created by a “tummy tuck.” The scar that results on the breast will depend upon the technique used for mastectomy.
Stacked-DIEP Flap is an innovative approach for women who thought they are too thin to have a breast reconstructed using their abdominal tissue
The Stacked-DIEP flap, also called a double DIEP, allows a breast to be reconstructed with significantly more tissue than can be obtained with either a single DIEP flap or a TRAM flap. This sophisticated microsurgical procedure can be an option, for example, for a thin woman who needs reconstruction of only one breast. Women who have been told that they are not candidates for a TRAM flap or a DIEP flap because they “do not have enough tissue” or because they have a vertical midline scar may be candidates for a stacked-DIEP flap reconstruction.
The Stacked-DIEP flap procedure uses two DIEP flaps (one DIEP flap from each side of the abdomen) to reconstruct a single breast. As is the case for all perforator flaps used in breast reconstruction, no muscle is sacrificed with this procedure. After the tissue is transferred to the chest, the blood vessels that supply the tissue of each of the flaps are connected to vessels at the recipient site using microsurgical techniques. The two flaps are then “stacked” and sculpted to restore the breast removed by mastectomy. Recovery is the same as it would be for any abdominal perforator flap.
Muscle Preserving Surgery
The blood vessels that are used for Stacked DIEP flap breast reconstruction are meticulously dissected without removing or destroying the muscle of the abdomen. Because muscle is preserved, postoperative pain and discomfort are minimized, and strength and function are preserved. After Stacked DIEP flaps are transferred to the chest, the blood vessels that will nourish the two DIEP flaps are connected to blood vessels at the mastectomy site using delicate microsurgical techniques. When possible, sensory nerves may also be connected to facilitate recovery of sensation in a reconstructed breast. Finally, the skin and fat of the Stacked DIEP flaps are shaped into a new breast.
Abdominal Contouring
Because the tissue removed from the lower abdomen during Stacked DIEP flap breast reconstruction surgery is similar to that removed during a tummy-tuck, women who undergo this procedure generally benefit from an improvement in the contour of their abdomen. While typically not as low as the scar of a tummy-tuck, the scar that results following Stacked DIEP flap surgery can typically be concealed in most clothing and in a once-piece bathing suit.
Optimizing Aesthetics
Approximately three months after the initial stage of breast reconstruction surgery, refinement of breast shape and procedures to produce overall symmetry can be completed. These optional additional procedures are performed on an outpatient basis and are referred to as Stage II.
Stacked DIEP Flap Breast Reconstruction in New York and Connecticut
Contact us if you would like more information about the options for breast reconstruction after mastectomy or to schedule a consultation. Our practice has offices in New York City and Greenwich, Connecticut.
Perforator Flap Procedures

Natural Tissue Breast Reconstruction with Perforator Flaps
Perforator flaps represent the current state-of-the-art in natural tissue breast reconstruction. Depending on the shape of your body and your personal preference, several areas of the body can act as donor sites for the tissue needed to restore the shape and form of the breast.
Perforator flap options for breast reconstruction include:
Using an incision similar to that used for a “tummy tuck,” skilled surgeons can reconstruct a breast from skin and fatty tissue taken from the lower abdomen—without removing any muscle.
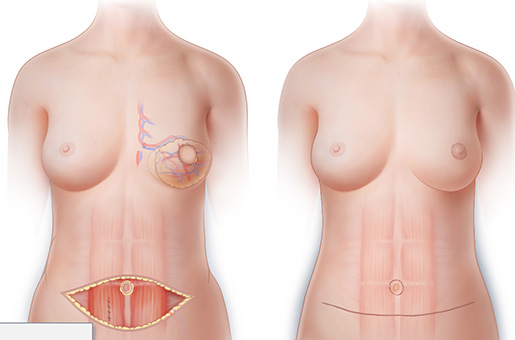
This innovative procedure uses two DIEP flaps, one DIEP flap from each side of the abdomen, to reconstruct a single breast. The Stacked-DIEP flap allows a single breast to be reconstructed with significantly more tissue than is possible using either a DIEP flap or a TRAM flap.
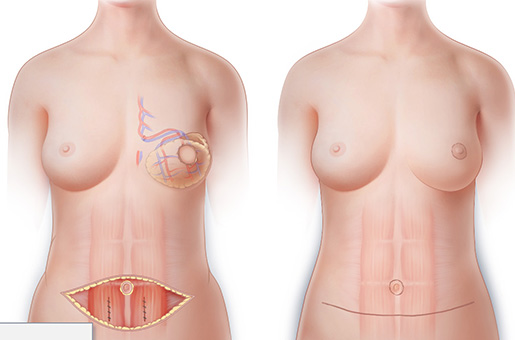
BODY LIFT BREAST RECONSTRUCTION WITH EXTENDED DIEP FLAPS
When there is not enough lower abdominal tissue to reconstruct both breasts to the desired size, the tissue of the flanks, hips or upper buttocks can be combined with tissue of the lower abdomen to achieve results not possible with ordinary perforator flaps.
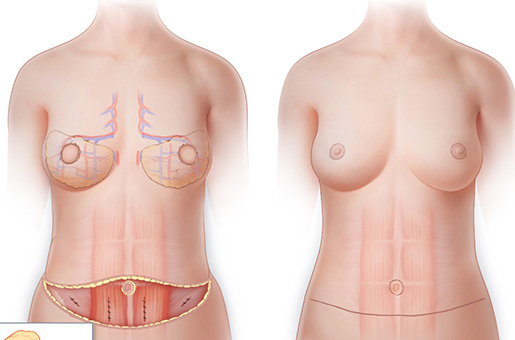
Similar to DIEP flaps, in that they use skin and fat from the lower abdominal area for breast reconstruction, SIEA flaps allow for breast reconstruction using lower abdominal tissue without muscle destruction.
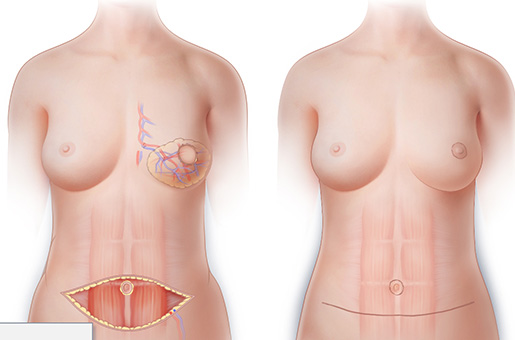
Using tissue fatty tissue from the “love-handle” area, is possible to reconstruct a woman’s breasts and at the same time, sculpt the lower back and lift the buttock.
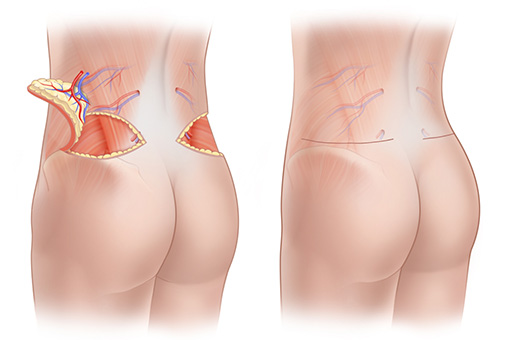
THE THIGH AS A DONOR SITE: PAP, DUG AND TUG FLAPS
The skin and fat of the upper thigh can also be used to reconstruct breasts with a natural appearance. Depending on the shape of the thigh and the distribution of fatty tissue, a PAP flap, DUG flap or TUG flap may be most appropriate.
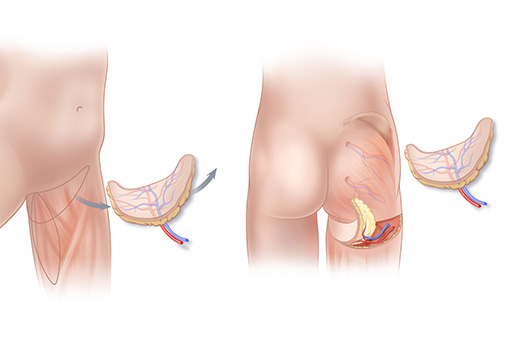
For women who cannot use—or choose not to use—tissue from their abdomen, lumbar area, or thighs, SGAP and IGAP flaps are an alternative for natural-tissue breast reconstruction after mastectomy. Without removing any muscle tissue can be borrowed from the upper (SGAP) or lower (IGAP) buttock.
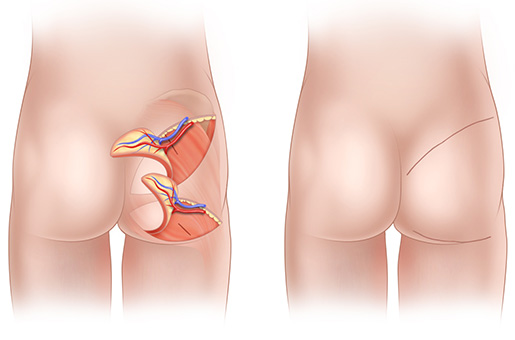
The Thoracodorsal Artery Perforator flap, known as a TDAP or TAP flap, is a perforator flap that can be rotated from the upper back to the chest for use in breast reconstruction.
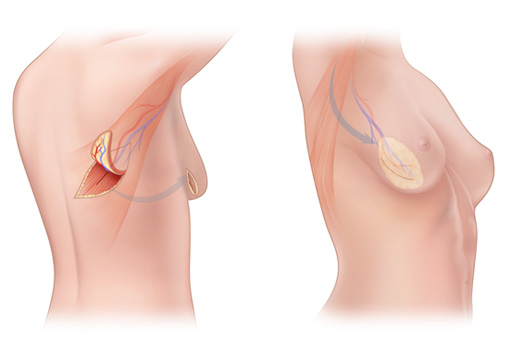
Nipple-Sparing Mastectomy

NIPPLE-SPARING MASTECTOMY

Nipple-sparing mastectomy preserves the nipple, areola and breast skin, and therefore enables the most natural-looking outcomes following breast reconstruction. Several different incisions can be used for nipple-sparing mastectomy. The optimal incision will depend upon many factors including breast size, patient preference, surgeon preference and the reconstructive plan. Several of the more commonly used incisions for nipple-sparing mastectomy are illustrated.

There are a variety of methods of nipple reconstruction; one commonly utilized method of autologous tissue nipple reconstruction is illustrated here. (A) The skin and fat that will form the projected nipple are surgically lifted from the breast reconstruction. (B) The tissue is brought together to form a nipple, and all incisions are closed with dissolvable stitches. (C) The nipple reconstruction is completed. Once the nipple has fully healed, tattooing can be used to shade the nipple and restore the appearance of the areola (not shown).
Women considering mastectomy to treat breast cancer or for risk reduction (prophylactic mastectomy) may be candidates for innovative procedures that can significantly improve the appearance of their reconstructed breasts. Nipple-sparing mastectomy (NSM) or as it is also known, nipple-preserving mastectomy, though not presently as widely performed as skin-sparing mastectomy, is the most cutting-edge technique of mastectomy presently available.
NSM removes the breast gland, but allows a woman to keep her nipple and areola in place. NSM is intended to improve cosmetic outcomes following mastectomy without compromising cancer care or the effectiveness of risk reduction surgery.
When appropriate oncologic and aesthetic criteria are strictly applied, NSM has the potential to allow women to preserve their nipples and areolas (the areola is the pigmented area surrounding the nipple) and enjoy the best possible cosmetic results following mastectomy and immediate breast reconstruction.
While there is still some debate about NSM in the medical community, an ever growing number of studies published in peer-reviewed journals including the Annals of Surgery, Annals of Surgical Oncology, The Breast Journal, Journal of Clinical Oncology, and Plastic and Reconstructive Surgery suggest that NSM can be safely performed in carefully selected patients. While not all women are candidates for NSM, the procedure may be appropriate for the treatment of certain breast cancers as well as for women undergoing prophylactic mastectomy.
Nipple-sparing mastectomy, is more difficult to perform than skin-sparing mastectomy because a breast surgeon must remove the ductal tissue directly behind the nipple, yet preserve sufficient blood supply to the skin and nipple and not leave breast tissue behind. For this reason, it is important that women considering nipple-sparing mastectomy choose a breast surgeon with experience in this cutting-edge procedure in order to assure both oncologic and cosmetic success.
Like all surgical procedures, NSM has benefits and risks. A woman considering this procedure must discuss it carefully with the members of her breast management team and make a choice that best suits her individual needs. Though the cosmetic benefits of keeping one’s own nipple and areola are readily apparent, women who are considering NSM must be aware of the potential risks of the procedure. In situations where NSM is either not recommended or desired, a Skin-Sparing Mastectomy is almost always an excellent option that can provide excellent cosmetic results.
Nipple-Sparing Mastectomy in Connecticut & New York
Our practice specializes in the most sophisticated techniques of natural-tissue breast reconstruction. When combined with nipple-sparing mastectomy, perforator flaps such as the DIEP flap, the SGAP flap and the SIEA flap can be used to restore the form of a woman’s breasts with healthy, warm living tissue; such reconstructed breasts may appear almost indistinguishable from those removed by mastectomy. We work closely with breast surgeons who are experienced at performing nipple-sparing mastectomies.
Lymphedema

Lymphedema After Breast Cancer Treatment
Women who have been or will be treated for breast cancer may be at risk of developing arm, breast, and chest swelling called lymphedema. Lymphedema occurs when lymph fluid that cannot be properly drained builds-up and causes swelling. Most women will not develop this side effect, but unfortunately, many will.
A network of lymph vessels collect watery, clear lymph fluid from the tissues of our body, much like veins collect blood. Lymph fluid is made up of proteins, water, salts and cells of the immune system. This fluid is carried to lymph nodes - small collections of tissue which act like filters and contain white blood cells that help us fight infection.
When one or more lymph nodes are removed as occurs during a sentinel lymph node biopsy or an axillary lymph node dissection, the way the lymph fluid flows in that side of the upper body is changed. These changes make it harder for fluid in the chest, breast, and arm to flow out of this area. If the remaining lymph vessels and lymph nodes cannot sufficiently compensate for those that were removed, excess fluid builds up and causes the swelling known as lymphedema. When lymphedema develops, it typically does so slowly over time. Patients who experience a sudden marked increase in swelling should be checked by their breast surgeon to evaluate for possible recurrence of tumor or disease.
All women who have lymphedema are advised to take some simple precautions to help control swelling, reduce complications and prevent long-term changes in the tissues that occur in response to chronic fluid build-up.
How is Lymphedema Treated
Treatment varies depending upon the severity of lymphedema. The available treatments for lymphedema can be divided into two categories - medical and surgical.
Medical Treatment of Lymphedema
The goals of lymphedema treatment are to reduce swelling, prevent swelling from getting worse, and decrease the chances of complications. Standard medical (non-surgical) treatment usually involves Manual Lymphatic Drainage (MLD), a type of medical massage designed to move the accumulated fluid out of the affected hand and arm. Complete Decongestive Therapy (CDT) combines MLD with meticulous skin care and hygeine, exercises, bandaging and the use of a specially fitted compression sleeve or stocking. Treatments are usually prescribed by a woman’s breast surgeon or oncologist and are performed by an experienced physical therapist with special training in lyphedema therapy.
While these techniques can be effective, they are can also be uncomfortable, inconvenient, and time-consuming. Strict compliance is essential, and since these treatments are palliative and not curative, treatment lasts a lifetime. When lyphedema is not controlled with standard treatments, surgery may offer relief.
Surgical Treatment of Lymphedema
Historically, surgical treatment of lymphedema was often ineffective, produced grotesque deformity and had horrific associated complications.
Superior surgical treatments are now, however, available to help treat patients with lymphedema. Vascularized Lymph Node Transfer and Lymphaticovenous Anastamosis, palliative but not curative procedures, offer hope to women with lymphedema.
Vascularized lymph node transfer can be performed as an isolated procedure or combined with a breast reconstruction procedure such a DIEP flap. This microsurgical procedure transfers a subset of lymph nodes from a low-risk lymph node basin to a limb with symptomatic lymphedema. The lymph nodes are transferred as a flap to the armpit or wrist of the affected extremity. Blood flow is re-established in the lymph node flap by attaching, with the aid of an operating room microscope, the blood vessels of the flap to blood vessels found in the recipient site.
Lymphaticovenous anastamosis or lymphaticovenular bypass was initially described over two decades ago as a means of treating lymphedema. More recently, “supermicrosurgical” modifications to the original procedure have been made to improve upon the original procedure. With the help on an operating room microscope and specially designed instruments, it is possible to divert blocked lymphatic vessels into the circulatory system by connecting them to tiny blood vessels called venuoles. Bridges established in this way allow drainage of lymphatic fluid into the vascular system.
These reconstructive procedures may be an attractive option for women when medical treatment options do not provide adequate relief of symptoms of lymphedema.
» Find out if you are a possible candidate for surgical lymphedema treatment
LAP Flap

LAP Flap Breast Reconstruction
Lumbar Artery Perforator Flap
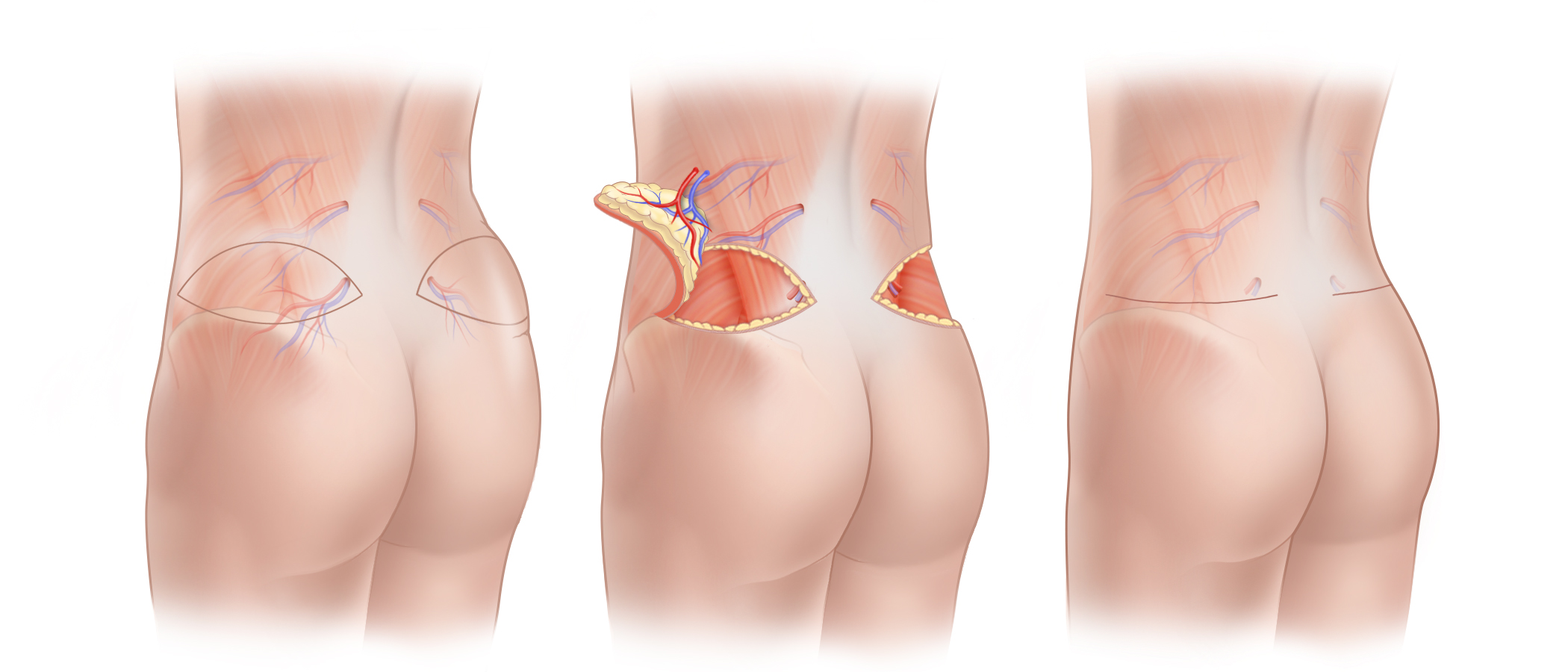
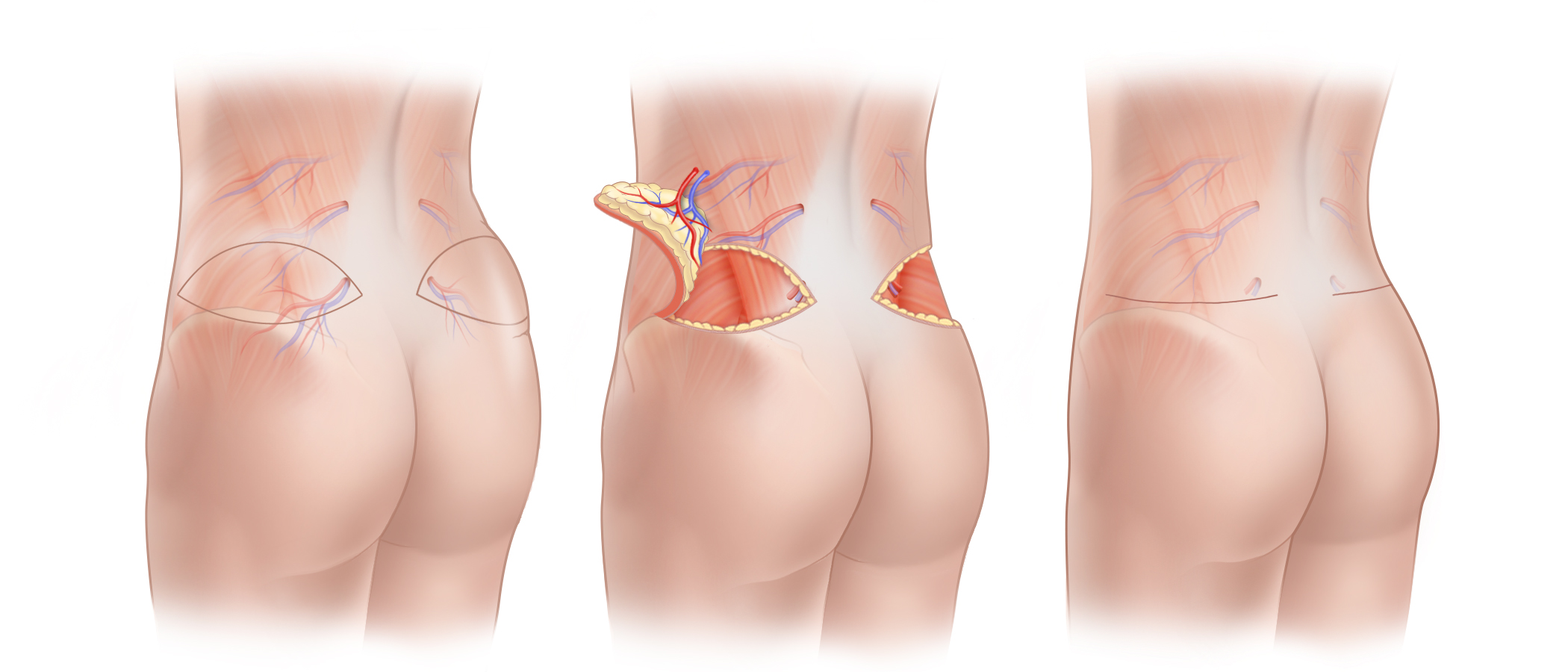
(A) A lumbar artery perforator flap (LAP flap) uses the soft tissue of the waistline at the lower back and the flank (the “love-handle” area) to reconstruct a breast. (B) A LAP flap is shown here being surgically elevated; as is the case with all perforator flaps, muscle remains intact at the flap’s donor site. Because of the location from with tissue is borrowed, LAP flap surgery lifts the buttock and contours the waistline. (C) The scar that results from harvest of a LAP flap lies along the waistline at the junction of the lower back and buttock where it can be concealed by most clothing and bathing suits. Once removed from the donor site, a LAP flap is transferred to the chest (not shown) and blood flow to the newly reconstructed breast is established using microsurgical techniques. The scar that results on the breast will depend on the technique of mastectomy. When just one breast is reconstructed with a LAP flap, the opposite side of the lower back is contoured to produce symmetry.
(A) A lumbar artery perforator flap (LAP flap) uses the soft tissue of the waistline at the lower back and the flank (the “love-handle” area) to reconstruct a breast. (B) A LAP flap is shown here being surgically elevated; as is the case with all perforator flaps, muscle remains intact at the flap’s donor site. Because of the location from with tissue is borrowed, LAP flap surgery lifts the buttock and contours the waistline. (C) The scar that results from harvest of a LAP flap lies along the waistline at the junction of the lower back and buttock where it can be concealed by most clothing and bathing suits. Once removed from the donor site, a LAP flap is transferred to the chest (not shown) and blood flow to the newly reconstructed breast is established using microsurgical techniques. The scar that results on the breast will depend on the technique of mastectomy. When just one breast is reconstructed with a LAP flap, the opposite side of the lower back is contoured to produce symmetry.
“Love Handles” Can Be Used To Reconstruct A Breast
Using tissue from the region just above the buttock to reconstruct the breasts can be an excellent option when personal preference, the shape of one’s body or a history of prior surgery make this area a more appealing donor site. Using Lumbar Artery Perforator (LAP) flaps, it is possible to reconstruct a woman’s breasts with soft tissue harvested from the lower back and hip—“love-handle”—areas. Since excess skin and fatty tissue are removed along the waistline, similar to that which is removed during cosmetic buttock-lift surgery, the buttocks end up in a higher position with these procedures. The scar that results from harvest of a LAP flap can generally be well concealed along the waistline where the buttock and lower back meet making this an appealing option for many women.
Muscle Preserving Surgery
The blood vessels that are needed for a LAP flap are meticulously dissected without removing any muscle. Since muscle is neither divided nor removed when harvesting a LAP flap, postoperative discomfort is minimized. After a LAP flap is transferred to the chest, the blood vessels of the flap are connected to blood vessels at the mastectomy site using an operating room microscope. The skin and fat of the LAP flap are then shaped into a new breast.
Optimizing Aesthetics
Approximately three months after the initial stage of breast reconstruction surgery, reconstruction of your nipples (when mastectomy includes their removal), refinement of breast shape and procedures to produce symmetry with your untreated breast can be completed. These optional additional procedures are performed on an outpatient basis and are referred to as Stage II.
Waistline Contouring
Because the tissue used for lumbar artery perforator flap breast reconstruction is similar to that removed during a buttock lift, women who undergo this procedure generally experience an improvement in the contour of their waistline and experience a degree of buttock lift. When just one breast is reconstructed using a LAP flap, tissue can be removed from the opposite side of the body to produce symmetric contours of the waistline and buttock. The scars that result from this type of surgery can typically be concealed in most clothing and in a one-piece bathing suit.
LAP Flap Surgery in New York and Connecticut
Contact us if you would like more information about LAP flaps for breast reconstruction or for information about other options for breast reconstruction including DIEP flap surgery or breast reconstruction using breast implants after mastectomy. Our practice has offices in New York City and Fairfield County, Connecticut.
Nipple Reconstruction

Nipple Reconstruction
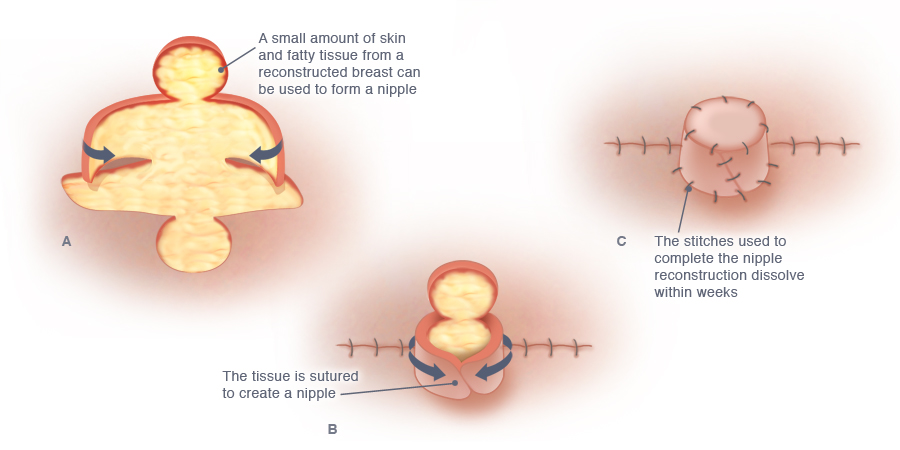
There are a variety of methods for nipple reconstruction; one commonly utilized method of nipple reconstruction is illustrated here. (A) The skin and fat that will form the projected nipple are surgically raised. (B) The surgically elevated tissue is brought together to form a nipple, and all incisions are closed with dissolvable stitches. (C) The nipple reconstruction is completed. Once the reconstructed nipple is fully healed, tattooing can be used to shade the nipple and restore the appearance of the areola (not shown).
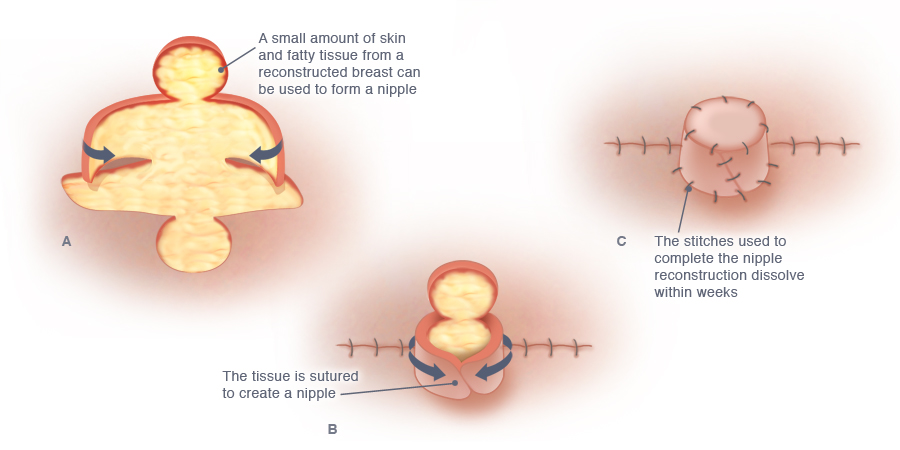
There are a variety of methods for nipple reconstruction; one commonly utilized method of nipple reconstruction is illustrated here. (A) The skin and fat that will form the projected nipple are surgically raised. (B) The surgically elevated tissue is brought together to form a nipple, and all incisions are closed with dissolvable stitches. (C) The nipple reconstruction is completed. Once the reconstructed nipple is fully healed, tattooing can be used to shade the nipple and restore the appearance of the areola (not shown).
Nipple reconstruction is usually performed as part of Stage II. Regardless of which method of breast reconstruction you chose, reconstruction of a nipple really makes a reconstructed breast look as normal and natural as possible. Because this minor procedure has a major impact on making a reconstructed breast look natural, most women choose the option of having nipples reconstructed.
A number of different techniques of nipple reconstruction can be used to reconstruct a nipple following natural tissue reconstruction. The best technique for you will depend on several factors such as the size of your breast, the shape of your breast, and the appearance of your other nipple if you have had only one breast reconstructed. Dr. Greenspun uses only your own tissue to provide projection to reconstructed nipples. At an outpatient visit about 6 to 8 weeks after surgery, the reconstructed nipple and the area around it are tattooed to fully restore the appearance of a normal nipple and areola.
Nipple Reconstruction in New York and Connecticut
Contact us if you would like more information about the options for nipple reconstruction after mastectomy or to schedule a consultation. Our practice has offices in New York City and Greenwich, Connecticut.
Breast Reconstruction with Perforator Flaps

Breast Reconstruction Using Your Own Tissue
Natural-tissue breast reconstruction methods use excess tissue from a woman’s own body to replace breast tissue removed by mastectomy.
- When tissue comes from your own body, it cannot be rejected by your immune system, and there is no need to worry about implant-specific issues such as implant rupture, capsular contracture, or the need for regular MRIs to monitor for “silent” implant leaks.
- Because living tissue used in breast reconstruction actually integrates with the tissue of the body, a breast reconstructed in this manner is typically warm, soft, and supple, and therefore tends to look and feel more natural than a breast reconstructed with a breast implant.
- Natural-tissue breast reconstruction has the potential for the reconstructed breast to develop sensation.
- Breasts reconstructed with a person’s own tissue will change in size with weight gain or loss, in proportion with rest of a person’s body.
One of the most important factors that differentiate flaps from one another is whether or not muscle is used in the breast reconstruction
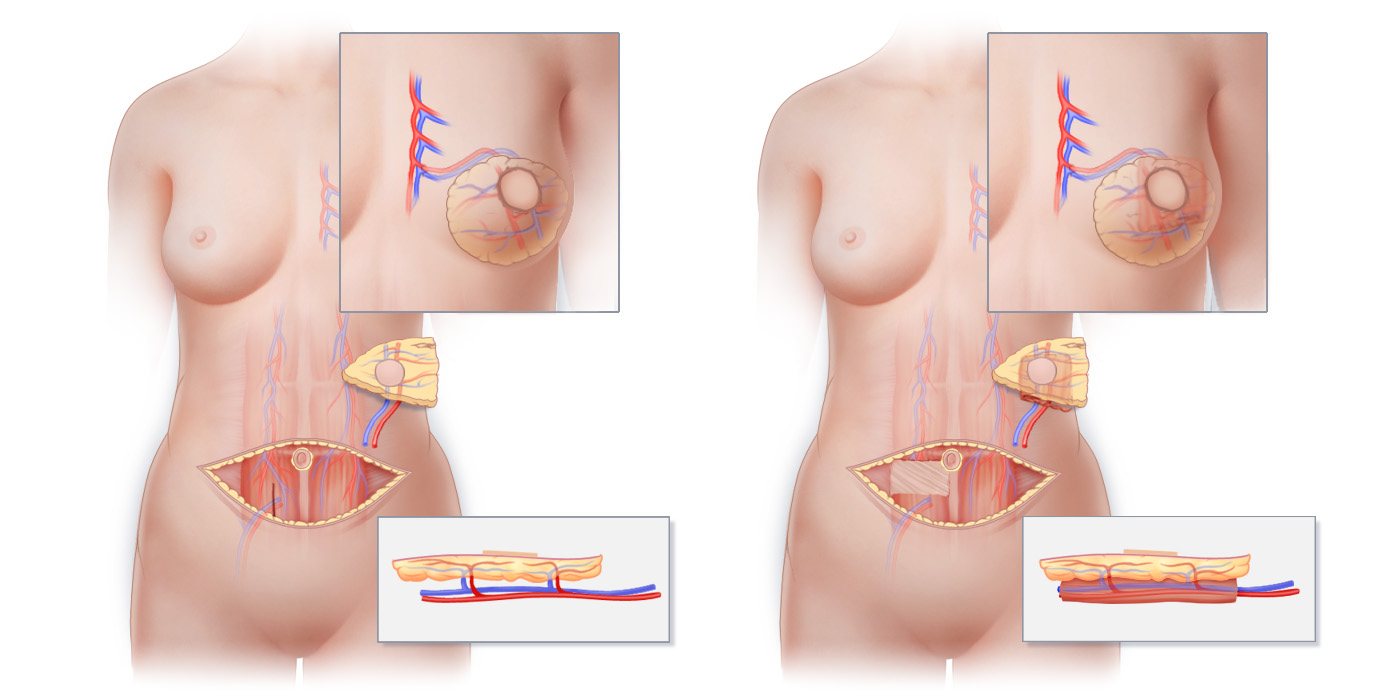
One of the most important factors differentiating various methods of natural-tissue breast reconstruction from one another is whether or not muscle is surgically removed from a flap’s donor site. Muscle does not grow back, so operations that remove muscle produce life-long changes that include weakness and increased risk for hernias. Perforator flaps such as the deep inferior epigastric perforator flap (DIEP flap) preserve muscle, while musculocutaneous flaps such as the free transverse rectus abdominus myocutaneous flap (free TRAM flap) remove portions of important muscles. (A) Preparation of a DIEP flap takes place without removing any muscle from the abdomen. (B) Preparation of a free TRAM flap requires removal of rectus abdominus muscle from the abdomen. Lower insets show flaps in cross-sectional view.
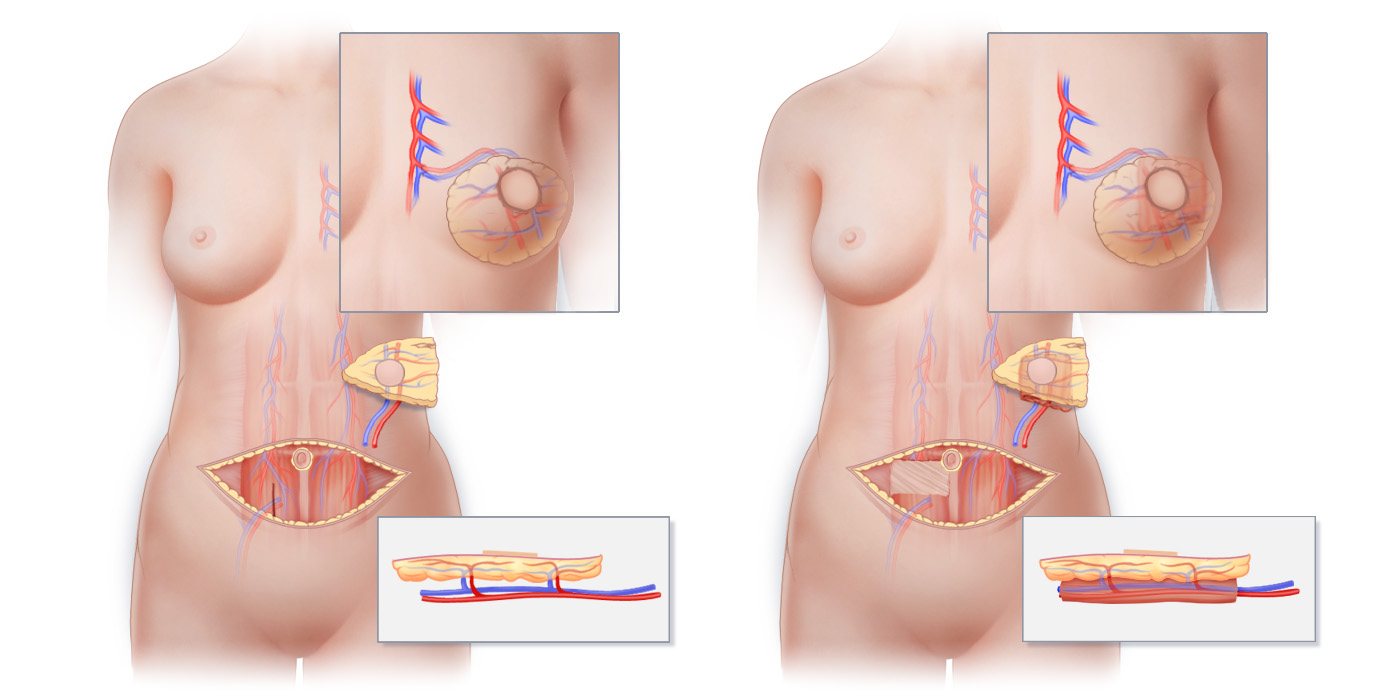
One of the most important factors differentiating various methods of natural-tissue breast reconstruction from one another is whether or not muscle is surgically removed from a flap’s donor site. Muscle does not grow back, so operations that remove muscle produce life-long changes that include weakness and increased risk for hernias. Perforator flaps such as the deep inferior epigastric perforator flap (DIEP flap) preserve muscle, while musculocutaneous flaps such as the free transverse rectus abdominus myocutaneous flap (free TRAM flap) remove portions of important muscles. (A) Preparation of a DIEP flap takes place without removing any muscle from the abdomen. (B) Preparation of a free TRAM flap requires removal of rectus abdominus muscle from the abdomen. Lower insets show flaps in cross-sectional view.
Perforator Flap Breast Reconstruction
Perforator flaps are the most sophisticated methods of natural-tissue breast reconstruction available. Perforator flaps do not contain muscle. This is an extremely important benefit in comparison to tissue reconstructions such as the TRAM flap and Latissimus flap that disrupt important muscles and weaken the body in the process.
Perforator flaps do not contain muscle.
In addition to giving you excellent cosmetic results without compromising important functional muscles, perforator-flap breast reconstruction offers several unique advantages:
- A more natural look and feel to reconstructed breasts than can typically be obtained with implants
- Less postoperative pain than is typically associated with reconstruction using flaps that include muscle
- Reconstructed breasts that will grow and shrink naturally as one’s weight changes, thereby keeping your reconstructed breast in proportion to your body
- Possible connection of sensory nerves in a perforator flap to nerves at the mastectomy site to help restore sensation to the reconstructed breast
- More rapid return to work and other activities than typically occurs following reconstruction with flaps that include muscle
- A significantly lower rate of unplanned reoperation (only 5%), as compared to the approximately 50% rate reported for implants 7 years after reconstruction
- Ability to reconstruct a breast after failure of an implant or other natural-tissue reconstruction, even after radiation
» Learn more about specific Perforator Flap Procedures
Microsurgical Breast Reconstruction
Advances in the field of microsurgery and the availability of sophisticated microsurgical techniques have revolutionized breast reconstruction surgery in recent years. In particular, when perforator flaps are used for reconstruction, skilled surgeons can shape tissue so that looks and feels as natural as a woman’s own breast. Perforator flap breast reconstruction offers the benefits of autologous breast reconstruction without the disadvantages of procedures that necessitate the sacrifice of muscle.
Our practice specializes in perforator flap breast reconstruction in Greenwich, Connecticut and New York City.
SIEA Flap

SIEA Flap Breast Reconstruction
Superficial Inferior Epigastric Artery Perforator Flap
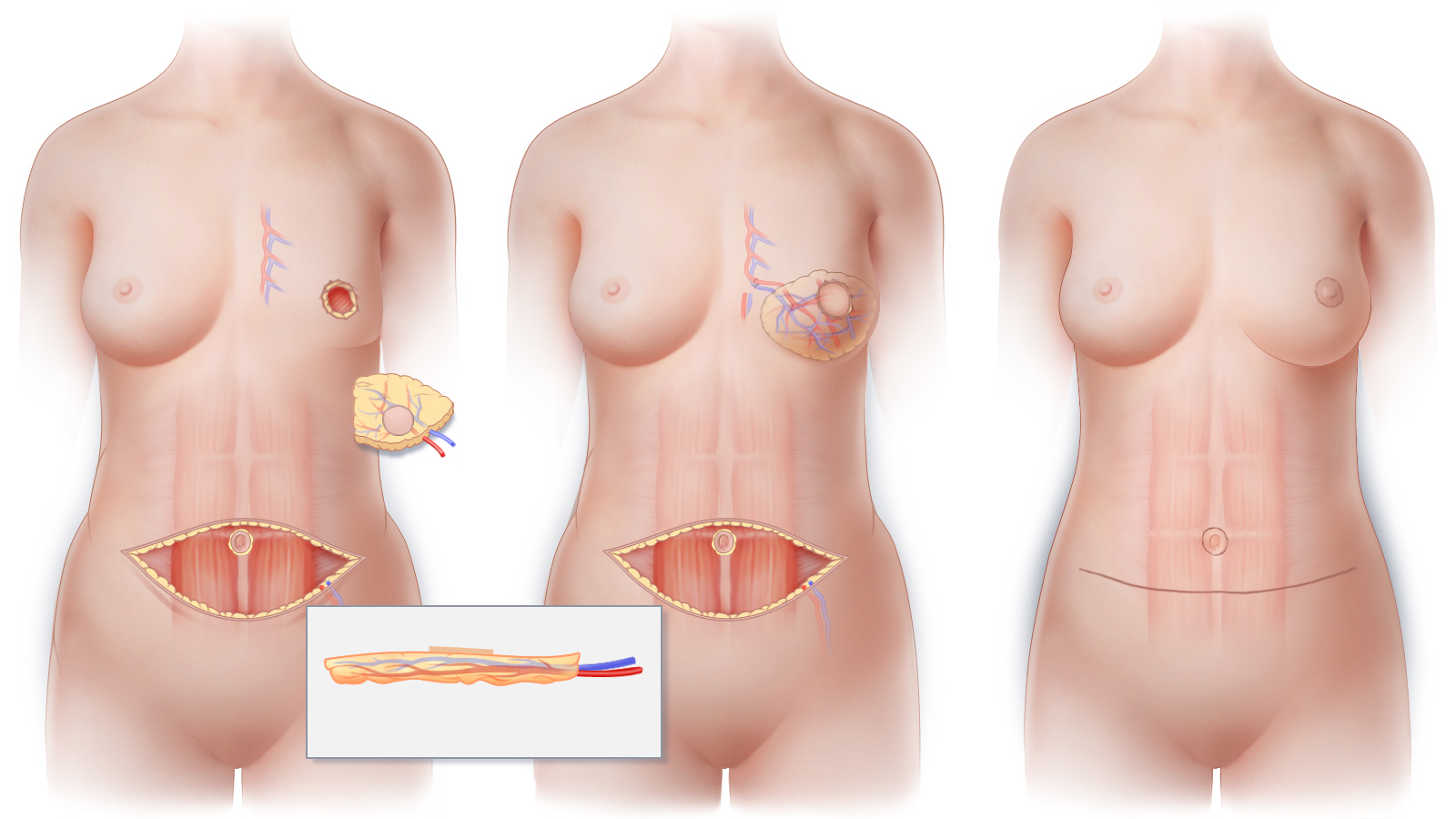
(A) The superficial inferior epigastric artery (SIEA) and the superficial inferior epigastric vein (SIEV) are the blood supply for the skin and fat of an SIEA perforator flap. These vessels travel in the fatty tissue just below the skin. (Inset) Cross-sectional view shows the SIEA and SIEV as they enter the flap directly. (B) The SIEA flap is transferred to the chest; using microsurgical techniques, the SIEA and SIEV are connected to blood vessels at the recipient site in order to restore circulation to the newly reconstructed breast. (C) The horizontal abdominal scar that results following SIEA flap surgery is similar to that created by a “tummy tuck” while the scar that results on the breast will depend on the technique used for mastectomy.
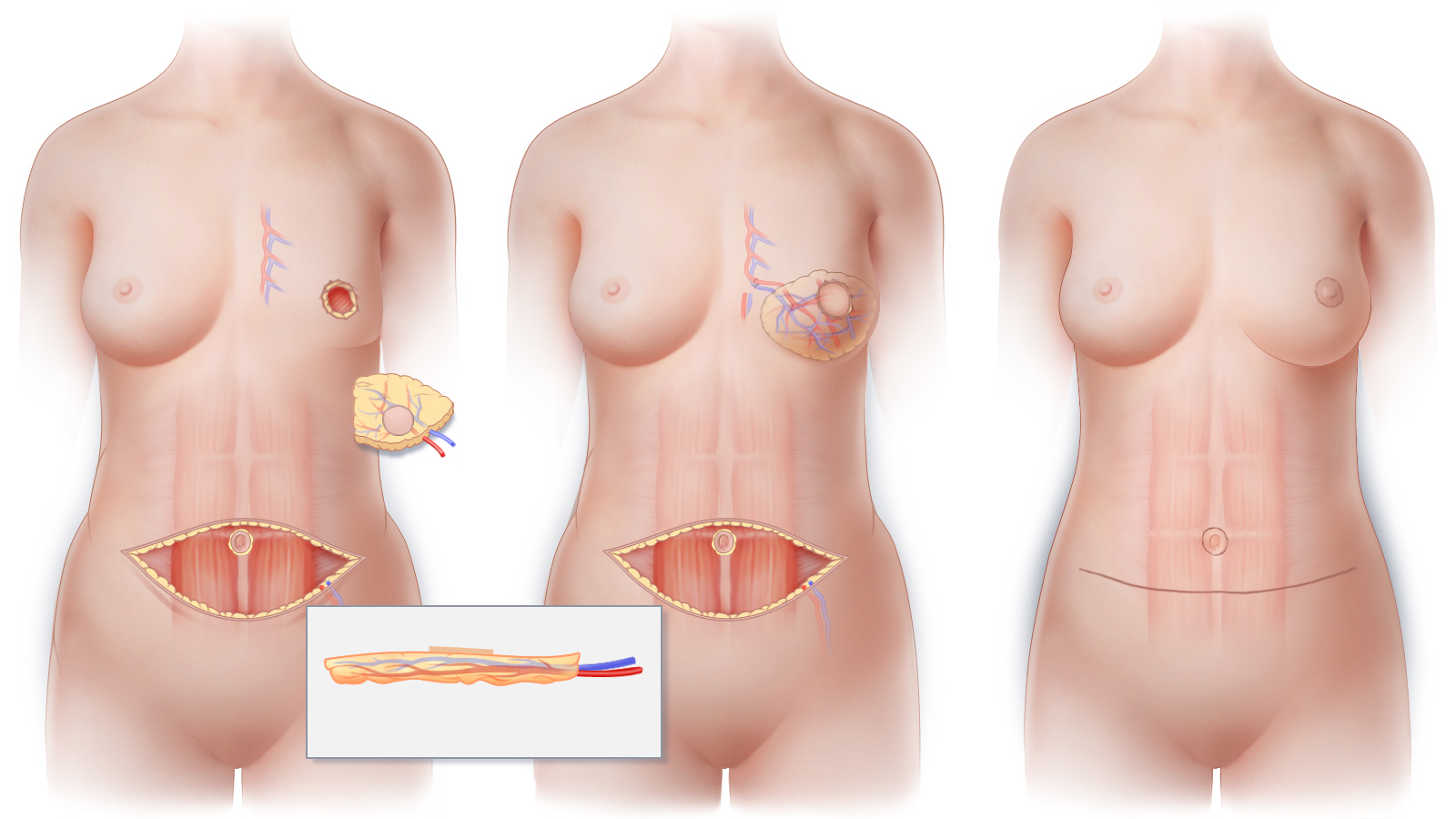
(A) The superficial inferior epigastric artery (SIEA) and the superficial inferior epigastric vein (SIEV) are the blood supply for the skin and fat of an SIEA perforator flap. These vessels travel in the fatty tissue just below the skin. (Inset) Cross-sectional view shows the SIEA and SIEV as they enter the flap directly. (B) The SIEA flap is transferred to the chest; using microsurgical techniques, the SIEA and SIEV are connected to blood vessels at the recipient site in order to restore circulation to the newly reconstructed breast. (C) The horizontal abdominal scar that results following SIEA flap surgery is similar to that created by a “tummy tuck” while the scar that results on the breast will depend on the technique used for mastectomy.
From a patient’s perspective, the DIEP and SIEA flaps are essentially indistinguishable.
Much like the DIEP flap, the SIEA flap employs the skin and fat of the lower abdominal area for breast reconstruction. After the incision is made for a lower abdominal perforator flap, the superficial inferior epigastric artery and vein are visible immediately beneath the skin. These vessels supply the skin and soft tissue of the abdomen and do not pass through the rectus abdominis muscle. In about 10% of women, these vessels are large enough to nourish the tissue needed for the breast reconstruction, and an SIEA flap can be performed.
As is the case for all perforator flaps used in breast reconstruction, no muscle is sacrificed with this procedure. After the tissue is transferred, blood vessels of the flap are connected to vessels at the mastectomy site using microsurgical techniques after which, the tissue of the SIEA flap is then sculpted into a new breast.
Abdominal Contouring
Because the tissue harvested from the abdomen during an SIEA is akin to that removed during a tummy-tuck, women who undergo this procedure generally benefit from an improvement in the contour of their abdomen. Since the scar on the lower abdomen that results from harvest of an SIEA flap is similar to that of a tummy-tuck, it can typically be concealed in most clothing.
Optimizing Aesthetics
Approximately three months after the initial stage of breast reconstruction surgery, reconstruction of your nipples (when mastectomy includes their removal), refinement of breast shape and procedures to produce symmetry with your untreated breast can be completed. These optional additional procedures are performed on an outpatient basis and are referred to as Stage II.
SIEA Flap Surgery in New York and Connecticut
Contact us if you would like more information about SIEA flap breast reconstruction or for information about other options for breast reconstruction after mastectomy including DIEP flaps. Our practice has offices in New York City and Fairfield County, Connecticut.
Breast Reconstruction with Breast Implants

Breast Reconstruction with Breast Implants
Breast reconstruction using breast implants is one of a number of different plastic surgery techniques that can be used to reconstruct a breast. Breast implants can be used to help recreate a breast removed by mastectomy, or to add volume to a breast significantly reduced in size following lumpectomy.
Of all of the techniques of breast reconstruction, reconstruction using breast implants generally requires the shortest hospital stay—often just overnight. In addition, when implants are used for reconstruction, scars can be limited to just the breast or breasts. For these and other reasons, breast reconstruction using breast implants, for many women, is the preferred approach to breast restoration, especially if they are able to have a one-stage implant reconstruction and avoid tissue expansion.
Reconstruction with breast implants is sometimes described as being “simple,” “straightforward” and/or the “least invasive” method of breast reconstruction. In some ways, these descriptions are accurate, however, they reflect a somewhat narrow view of what breast reconstruction means for each person. While an implant breast reconstruction may involve less initial surgery than a natural-tissue reconstruction, women who chose to have implant reconstructions have much higher rates of unplanned reoperations and reconstruction failures than do those who chose natural-tissue reconstructions.
Of course, since each method of breast reconstruction has specific advantages and disadvantages, the best procedure for your reconstruction will depend on many factors including your medical history, your breast cancer treatment plan, and most importantly, your personal preference and goals. The advantages of breast implant reconstruction should be weighed against the disadvantages, including a high rate of unplanned re-operation and the anticipated lifespan of breast implants. For women who wish to undergo restorative breast surgery without an implant, natural-tissue reconstructive procedures may be appealing.
Advantages of Breast Implant Reconstruction
The advantages of implant breast reconstruction over natural-tissue breast reconstruction include:
- Limiting your healing and surgical scars to the breast area alone
- Shorter initial surgery and hospital stay
- Slightly shorter initial recovery time
Implant breast reconstruction may be a good option if:
- You want to avoid having a scar on another part of the body.
- You want to have breast reconstruction with the shortest possible recovery time.
- You want to achieve a breast size that is larger than possible even with the latest “stacked” flap natural-tissue reconstruction options.
- You will not have or have not had radiation therapy. (Radiation therapy significantly increases the chances of developing significant problems with an implant reconstruction.)
- You are not healthy enough to undergo a natural-tissue reconstruction procedure.
Breast Implant Reconstruction Techniques
One-Step Prepectoral Implant Breast Reconstruction
In certain situations, a breast implant can be placed directly into the space created by mastectomy. This state-of-the-art approach, known as pre-pectoral implant reconstruction, allows some women to skip the tissue expansion process. When done in combination with nipple-preserving mastectomy, a breast can sometimes be fully reconstructed in a single surgical procedure.
To learn more about one-stage breast implant reconstruction, click here
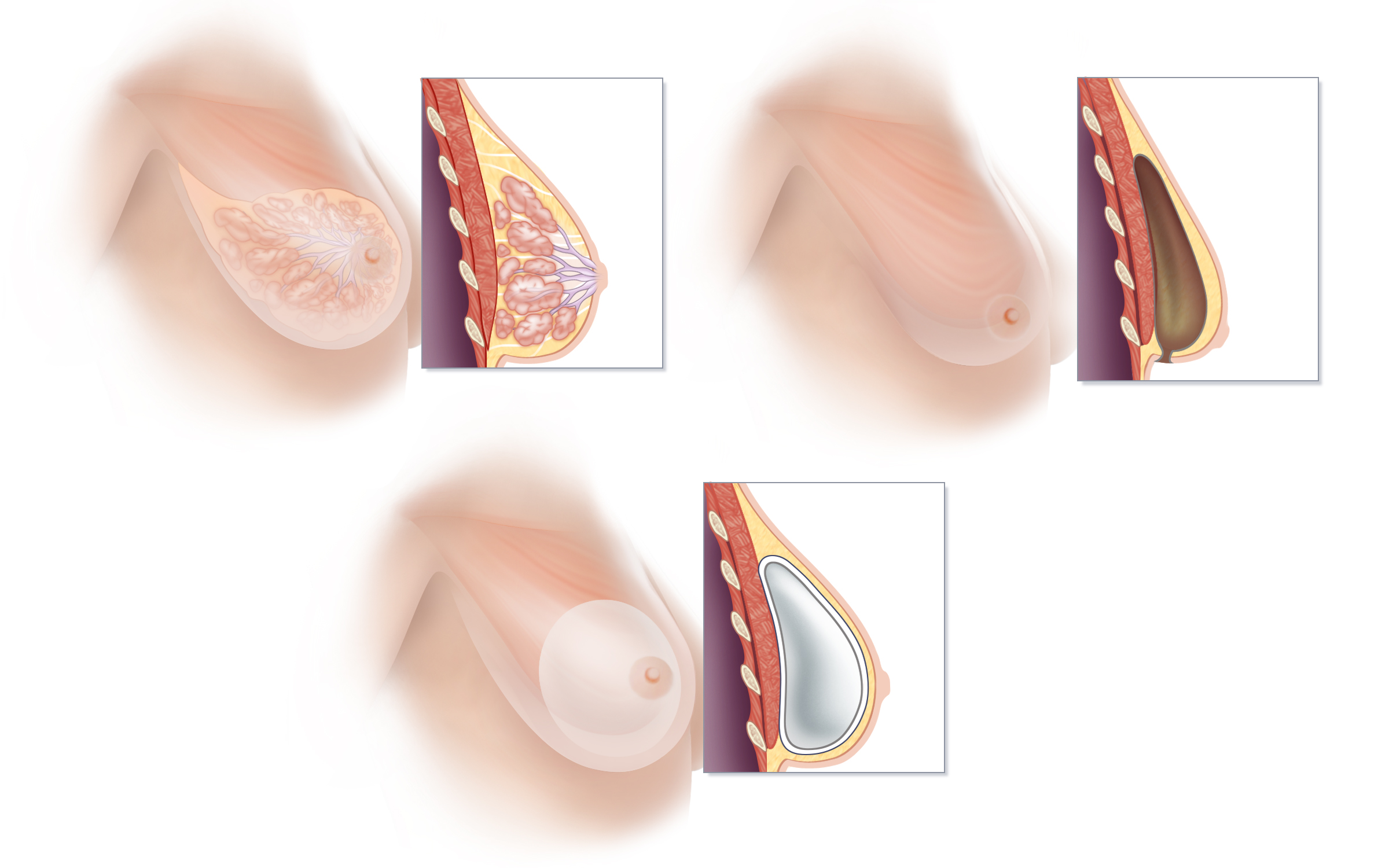
The current state-of-the-art approach to reconstruction using breast implants avoids damage to the pectoralis muscle that necessarily occurs with traditional tissue expander-implant breast reconstruction techniques. (A) Breast tissue is normally located just in front of the pectoralis muscle of the chest. (B) When breast tissue is removed by mastectomy, an empty space is inherently created between the pectoralis muscle and the breast skin. Prepectoral breast implant reconstruction takes advantage of this empty space. (C) Placing a silicone-filled implant wrapped in specialized acellular dermal matrix directly into the space that results at the time of mastectomy avoids the weakness and discomfort commonly reported with traditional breast implant reconstructions. The normal anatomy and function of the pectoralis muscle is preserved, and visible movement of the implant with muscle contraction—a phenomenon known as “animation deformity”—which occurs frequently with traditional under-the-muscle reconstruction, is avoided.
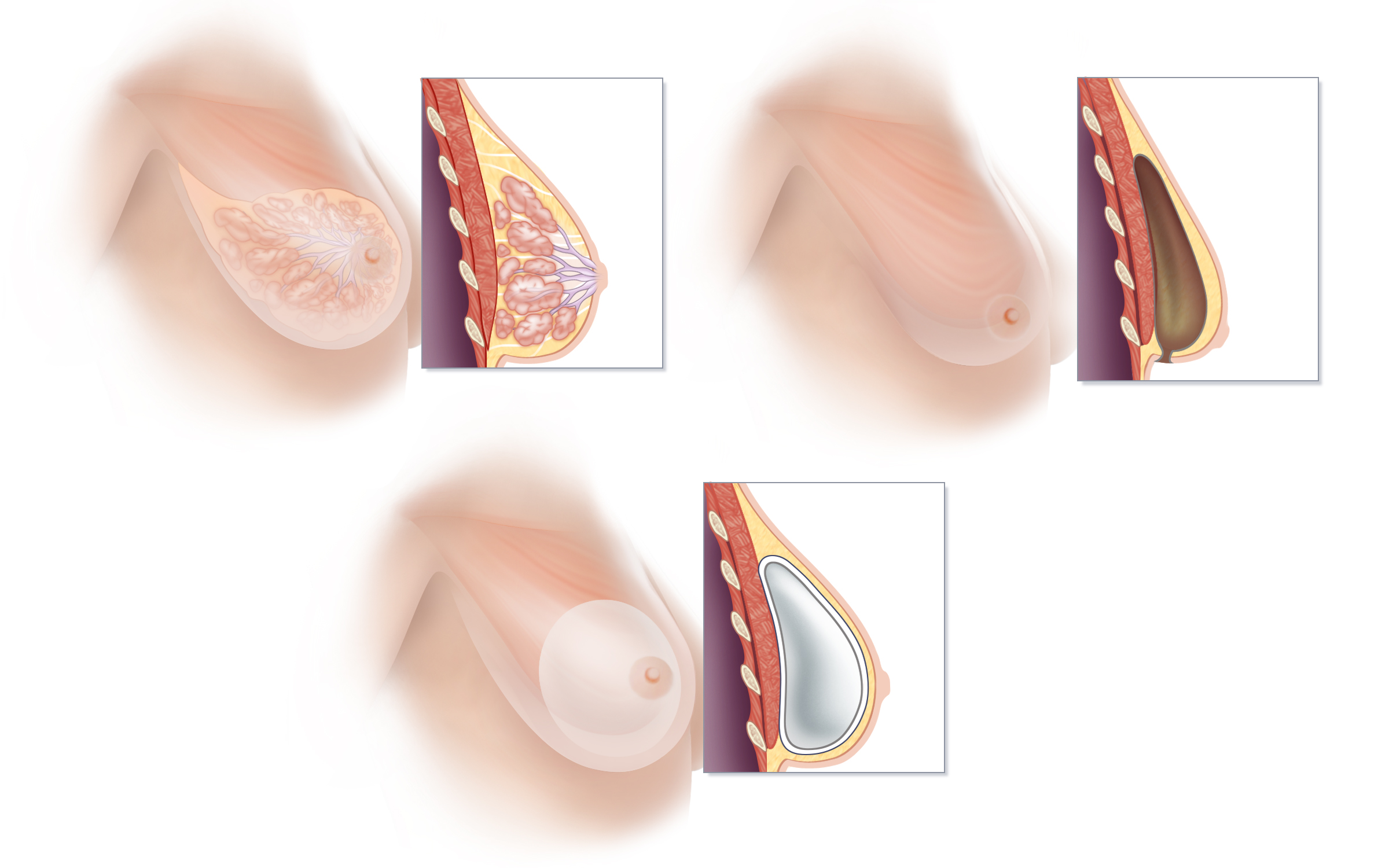
Tissue Expander/Implant Breast Reconstruction
Traditional implant reconstruction involves two or three surgical procedures, beginning, at the time of mastectomy, with the placement of a “tissue expander” under one of the muscles of the chest. The tissue expander is gradually inflated by adding air or fluid to the device over a period of weeks to months. At a second surgery, the tissue expander is removed, and a breast implant is placed.
To learn more about tissue expander/implant reconstruction, click here
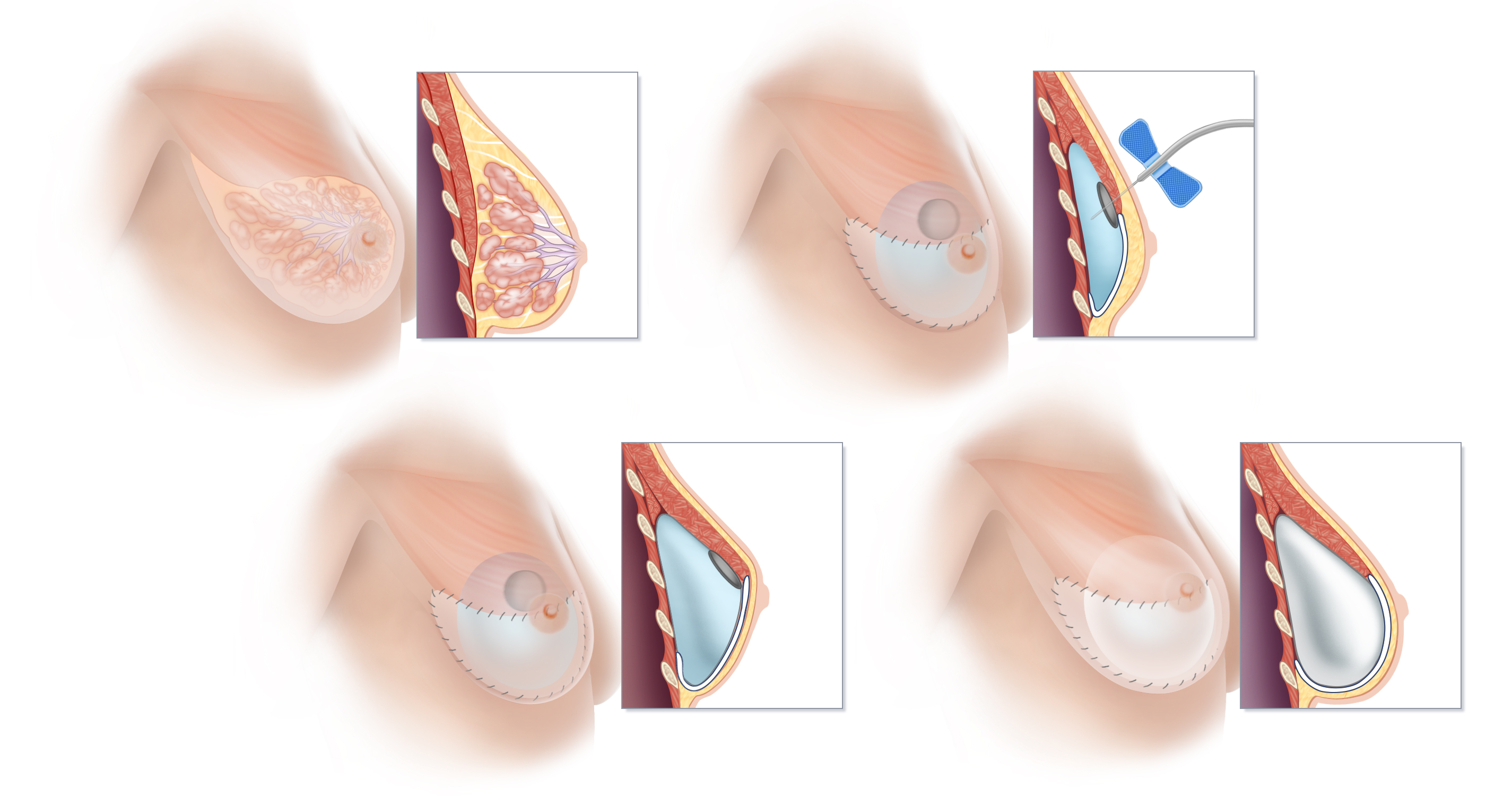
(A) Breast tissue is located on top of the muscles of the chest, between the pectoralis muscle and the skin. The lobules of the breast responsible for milk production drain into a system of ducts that travel to the nipple. If a woman’s reconstructive plan calls for a breast implant to be placed “under the muscle,” the pectoralis muscle must be stretched out to create ample space for the implant. In order to create this space, the lower edge of the pectoralis major is surgically separated from the chest wall, and a tissue expander is inserted beneath this muscle. The lower portion of the tissue expander is then typically covered with a specialized acellular dermal matrix to provided added support. (B) At each of a series of office visits following recovery from surgery, the tissue expander is gradually inflated by injection with sterile fluid or air. (C) Once the tissue expander is fully expanded and sufficient space created, an additional surgical procedure is scheduled to remove the expander and replace it with a breast implant. (D) Below the stretched-out pectoralis muscle, a breast implant has replaced the tissue expander. In many cases, the stretched muscle will cover only the upper portion of the implant, and more complete coverage of the breast implant is accomplished by using a tissue matrix such as AlloDerm or Dermacell® between the lower edge of the pectoralis muscle and the chest wall.
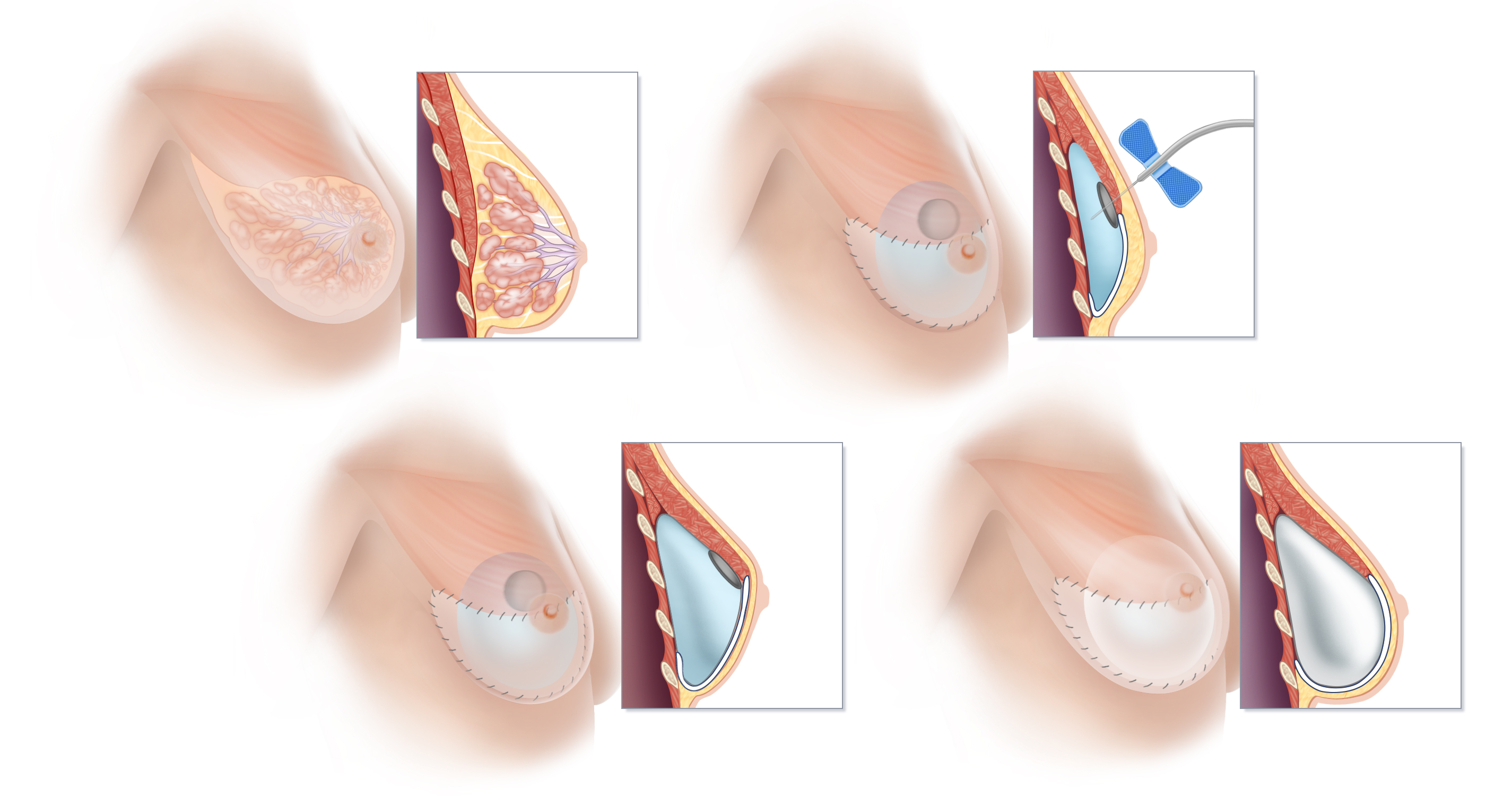
Breast Implant Breast Reconstruction in New York and Connecticut
Contact us to schedule a consultation, or if you would like more information about the options for breast reconstruction after mastectomy. Our practice has offices in Greenwich, Connecticut and New York. We perform breast reconstruction surgery at several hospitals in Connecticut and New York.
DIEP Flap

DIEP Flap Breast Reconstruction
Deep Inferior Epigastric Perforator flap
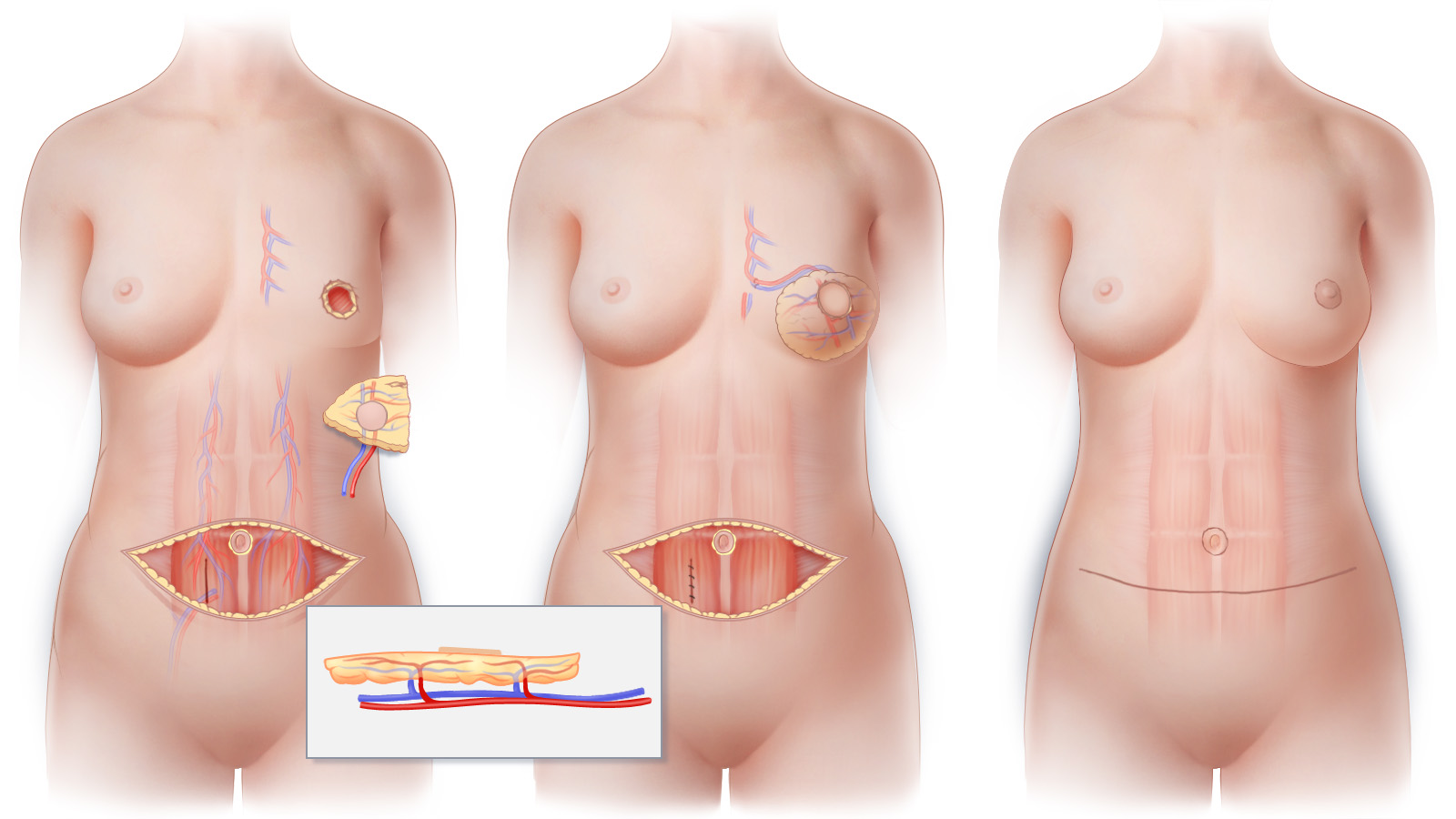
(A) By way of branches called perforators, the deep inferior epigastric artery (DIEA) and the deep inferior epigastric vein (DIEV) provide blood supply to the skin and fatty tissue of a DIEP flap. During the surgical preparation of the DIEP flap, these perforator blood vessels are meticulously separated from the abdominal muscle, leaving the muscle with enough remaining blood supply intact. (Inset) Cross-sectional view demonstrating perforator branches of the DIEA and DIEV that nourish the tissue of the DIEP flap. (B) To restore circulation to the tissue of the newly reconstructed breast after the DIEP flap is transferred to the chest, the blood vessels of the flap are connected to blood vessels at the recipient site using microsurgical techniques. The flap is then sculpted to restore the shape of the breast. (C) The horizontal abdominal scar that results following DIEP flap surgery is similar to that created by a “tummy tuck.” The scar that results on the breast will depend upon the technique used for mastectomy.
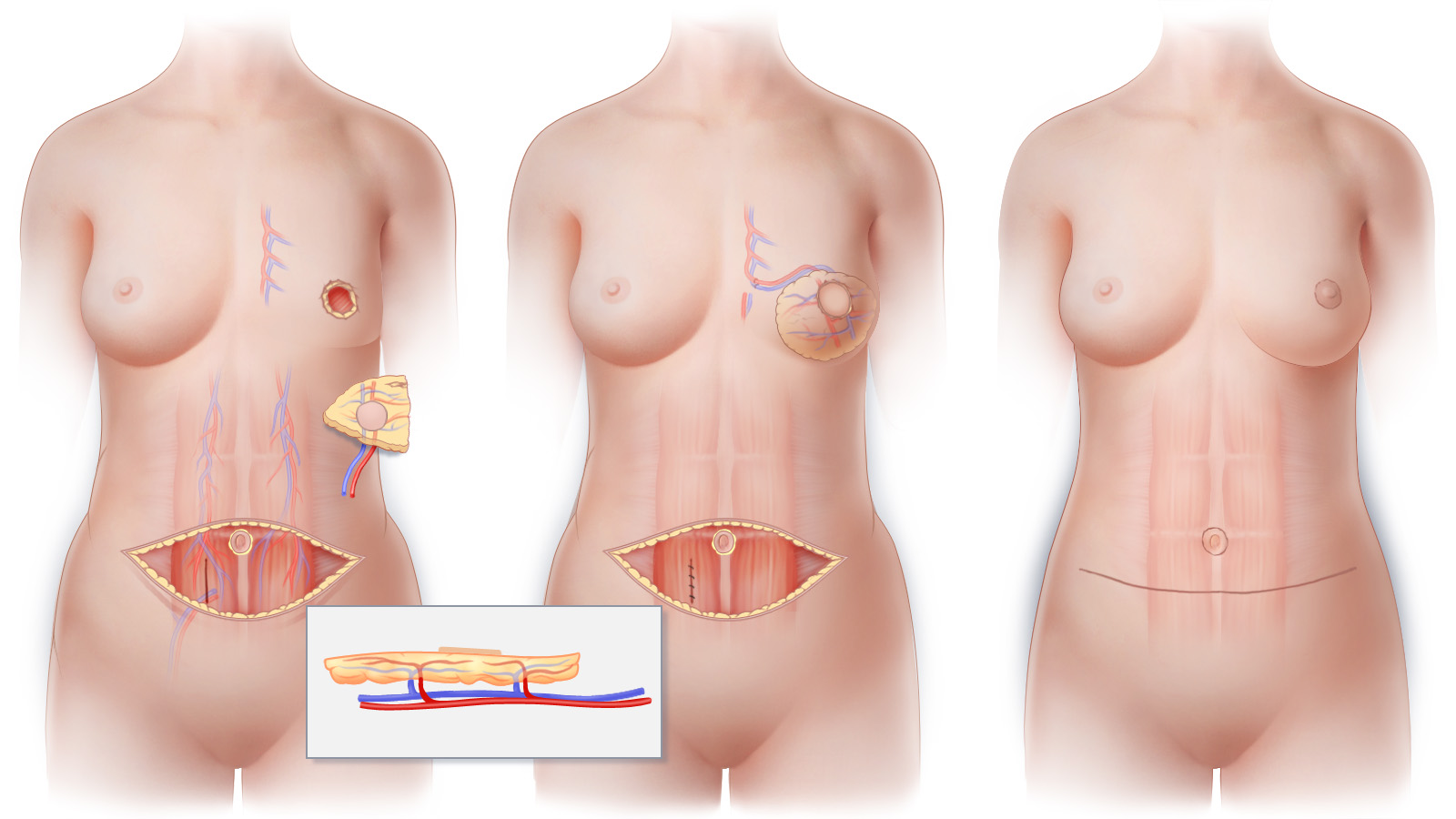
(A) By way of branches called perforators, the deep inferior epigastric artery (DIEA) and the deep inferior epigastric vein (DIEV) provide blood supply to the skin and fatty tissue of a DIEP flap. During the surgical preparation of the DIEP flap, these perforator blood vessels are meticulously separated from the abdominal muscle, leaving the muscle with enough remaining blood supply intact. (Inset) Cross-sectional view demonstrating perforator branches of the DIEA and DIEV that nourish the tissue of the DIEP flap. (B) To restore circulation to the tissue of the newly reconstructed breast after the DIEP flap is transferred to the chest, the blood vessels of the flap are connected to blood vessels at the recipient site using microsurgical techniques. The flap is then sculpted to restore the shape of the breast. (C) The horizontal abdominal scar that results following DIEP flap surgery is similar to that created by a “tummy tuck.” The scar that results on the breast will depend upon the technique used for mastectomy.
Muscle Preserving Surgery
The blood vessels that are needed for a DIEP flap breast reconstruction are meticulously dissected without removing or destroying the muscles of the abdomen. Because muscle is preserved, postoperative pain and discomfort are minimized, and strength and function are preserved. After DIEP flap is transferred to the chest, the blood vessels that will nourish the DIEP flap are connected to blood vessels at the mastectomy site using delicate microsurgical techniques. When possible, sensory nerves may also be connected to facilitate recovery of sensation in a reconstructed breast. Finally, the skin and fat of the DIEP flap are shaped into a new breast.
Abdominal Contouring
Because the tissue removed from the lower abdomen during DIEP surgery is similar to that removed during a tummy-tuck, women who undergo this procedure generally benefit from an improvement in the contour of their abdomen. While typically not as low as the scar of a tummy-tuck tuck, the scar that results from DIEP flap can typically be concealed in most clothing and in a once-piece bathing suit.
Optimizing Aesthetics
Approximately three months after the initial stage of breast reconstruction surgery, refinement of breast shape and procedures to produce overall symmetry can be completed. These optional additional procedures are performed on an outpatient basis and are referred to as Stage II.
DIEP Flap Breast Reconstruction in New York and Connecticut
Contact us to schedule a consultation, or if you would like more information about the options for breast reconstruction after mastectomy. Our practice has offices in Greenwich, Connecticut and New York. We perform breast reconstruction surgery at several hospitals in Connecticut and New York.
Click here to view photographs of women who have undergone reconstruction with DIEP Flaps
Treatment

BREAST CANCER TREATMENTS
Standard treatment for breast cancer usually includes one of more of these options:
Surgery
Almost all women diagnosed with breast cancer will undergo some form of surgery to remove the cancer. The various surgical treatment options—such as nipple-sparing mastectomy, oncoplastic surgery and lumpectomy—are described in this section.
Radiation Therapy
Radiation therapy is used to destroy cancer cells in the breast that may remain after surgery. In treating breast cancer, radiation is used routinely after lumpectomy and selectively after mastectomy, in order to help reduce the chances that the cancer will recur.
Chemotherapy
Chemotherapy is a type of cancer treatment that uses drugs to to slow or stop the growth of cancer cells. Chemotherapy, sometimes simply called “chemo,” may be used before surgery, after surgery or both. It is rarely, if ever, used as the only treatment for breast cancer.
Hormone Therapy
Certain hormones can promote the growth of some breast cancers. Hormone therapy can be used to slow or stop the growth of cancer cells that are sensitive to such hormones as estrogen.
Risk Factors

Breast Cancer Risk Factors
What Causes Breast Cancer?
No single cause of breast cancer has been identified. Both genetic and hormonal factors increase a woman’s risk factors for developing breast cancer.
Here are some of the factors that can increase the chances of developing breast cancer:
- Age (the chance of developing breast cancer increases as you get older)
- Previous cancer in either of your breasts
- A history of breast cancer in your family
- A history of ovarian cancer in your family
- Hereditary factors such as having the genetic abnormality known as BRCA1 or BRCA2
- A history of having had radiation to your chest (for example, in the treatment of Hodgkin’s Disease)
- Having had your first menstrual period before age 12
- Menopause after age 55
- Having your first pregnancy later in life
- Never having been pregnant
- Race (Caucasian women are at higher risk than African-American, Hispanic, Asian or Native American women)
- Ashkenazi Jewish heritage
- Being overweight
- Having a sedentary lifestyle
- Alcohol consumption (studies suggest that a woman’s risk of breast cancer goes up as alcohol consumption increases)
- Consumption of a high-fat-content diet
Genetics and Heredity

Genetics and Inherited Breast Cancer Risk
You have likely heard and read about a family tendency for certain diseases. A propensity for some diseases is, in fact hereditary. That’s why in a routine medical examination you’re likely to be asked if any of your close relatives has had diabetes, or heart disease, or cancer.
Genetics and Breast Cancer
For centuries, scientists have recognized that certain traits can be passed from parents to their offspring through genes. Genetics, the study of heredity, tells us that our genes carry the genetic code for various traits in the form of DNA. DNA directs the cells that make up our bodies how to behave. Genes determine not only inherited features such as eye color and height, but also the transmission of certain diseases such as sickle cell anemia and cystic fibrosis. While everyone has some chance of developing cancer, for example, the inheritance of some genes can place a person at significantly higher risk of developing certain types of cancer, including breast cancer.
Alterations in the genetic code––known as mutations–– can predispose those who inherit them to developing certain diseases. Scientists have identified a number of genetic mutations that can cause different kinds of cancer. Simple blood tests, such as the one for the BRCA1 and BRCA2 genes, can now be used to learn about a your genetic makeup, empowering you to make important choices and to take steps that may reduce your risk of developing cancer.
Federal Law Prohibits Discrimination Based Upon Genetics
Some people have been afraid to be tested for genetic diseases for fear that the information discovered can be used to deny them insurance. The Genetic Information Nondiscrimination Act of 2008 (P.L. 110-233, 122 Stat. 881), also referred to as GINA, is a new Federal law that prohibits discrimination in health coverage and employment based on genetic information.
GINA generally will prohibit discrimination in health coverage and employment on the basis of genetic information. GINA, together with already existing nondiscrimination provisions of the Health Insurance Portability and Accountability Act, generally prohibits health insurers or health plan administrators from requesting or requiring genetic information of an individual or the individual’s family members, or using it for decisions regarding coverage, rates, or preexisting conditions. The law also prohibits most employers from using genetic information for hiring, firing, or promotion decisions, and for any decisions regarding terms of employment.
Detection & Diagnosis

Detection and Diagnosis of Breast Cancer
Mammograms
In addition to seeing your doctor for routine examinations, it is important to discuss having routine screening mammograms, as an abnormal finding on a mammogram is frequently the first indicator of breast cancer in women without symptoms.
The American Cancer Society recommends that “women age 40 and older should have a screening mammogram every year and should continue to do so for as long as they are in good health.”
In the fall of 2009, the U.S. Preventive Services Task Force made headlines when it released a controversial recommendation that most women without symptoms of breast cancer should begin to have biannual screening mammograms at age 50. In spite of the Task Force’s recommendation, the American Cancer Society, the American College of Surgeons, the American College of Radiology and many other experts continue their strong recommendation that yearly screening mammograms begin at age 40.
How Is A Diagnosis of Breast Cancer Made?
If a mammogram or any other finding suggests that breast cancer might be present, a biopsy is necessary to make a diagnosis. A biopsy is a sample of tissue taken from the breast (or other site) and evaluated under a microscope and with special tests to determine if cancer cells are present. Sometimes a biopsy will involve a short outpatient surgical procedure, but in many cases the sample for a biopsy can be obtained in your doctor’s office using a needle without even making an incision.
Hereditary Breast Cancer

Heredity and Breast Cancer
Inherited Risk
Although most cases of breast cancer are thought not to be hereditary, genetic inheritance has been shown to play a role in many breast cancer cases. A family history of breast and/or ovarian cancer may indicate a hereditary risk for developing one or both of these cancers. For example, if a woman has a first-degree relative (mother, daughter or sister) who has had breast cancer, her chances of developing the disease may be 2 to 3 times higher than that of the general population. People who have themselves had breast or ovarian cancer, have a history of breast or ovarian cancer in their family, or are of Ashkenazi (Eastern European) Jewish heritage are more likely to carry genes that place them at increased risk for developing breast cancer.
Family History and Breast Cancer Risk
Although at present the most widely available laboratory testing for hereditary breast cancer analyzes the BRCA1 and BRCA2 gene mutations, a significant proportion of all hereditary breast cancer may be caused by mutations in genes other than BRCA1 and BRCA2. This means that, even when the BRCA1 and BRCA2 gene tests do not reveal any mutation, a woman with a strong family history of breast cancer (as well as certain other cancers) may carry other genetic mutations that place her at significantly higher than average risk for developing breast cancer.
If there have been cases of breast or ovarian cancer in your family, you may want to consider consulting a genetic counselor or a breast surgeon, and have genetic testing to help you learn both your specific risk and to better inform yourself as you make important choices about your medical care.
Contact us if you would like to make an appointment and learn more about your options.
Reconstruction vs. Augmentation

The Difference between Breast Reconstruction and Breast Augmentation
Although breast implants generally work well for cosmetic breast augmentation in women who have not undergone mastectomy, inherent problems with their use in breast reconstruction may make this kind of breast replacement a less desirable choice for many women.
Why is there such a difference when both procedures use implants? First, women who have implants placed for cosmetic breast enlargement have natural breast tissue that covers the implants and acts as a protective layer helping to prevent the capsule that invariably forms around an implant from being noticeable. When all of the breast tissue has been removed by mastectomy, only a thin layer of skin remains. The absence of breast tissue after mastectomy can make it more difficult to achieve a natural look and feel using breast implants. Second, since a synthetic implantable prosthesis has a fixed shape and cannot be sculpted, if a woman is having only one breast reconstructed with an implant, it may be difficult to achieve a satisfactory degree of symmetry with the natural breast. It is difficult to match an implant to the shape of the other breast’s natural tissue.
Although complications and unplanned reoperation also happen after cosmetic breast augmentation, they occur much less frequently than after implant reconstruction.
Oncoplastic Surgery

Oncoplastic Surgery and Partial Breast Reconstruction
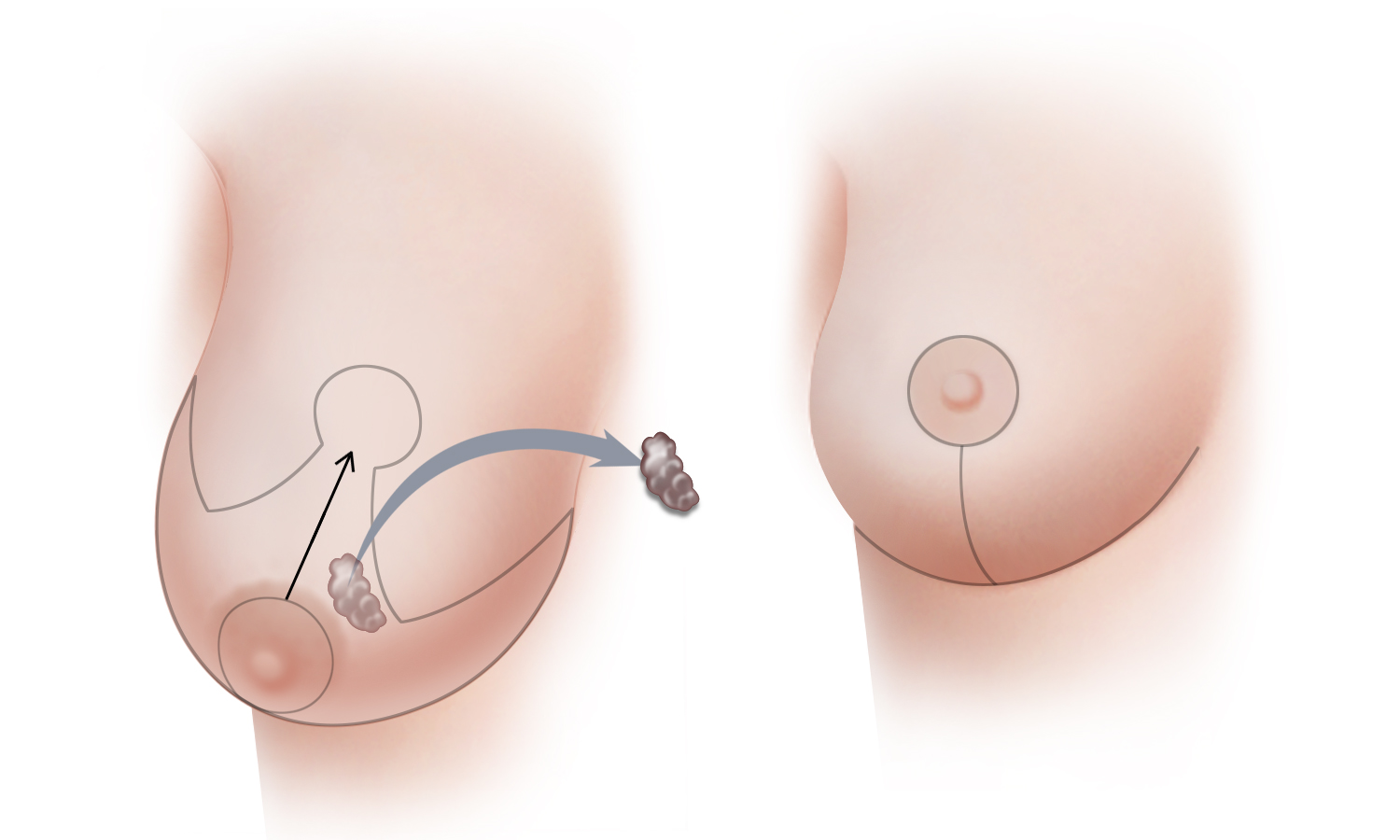
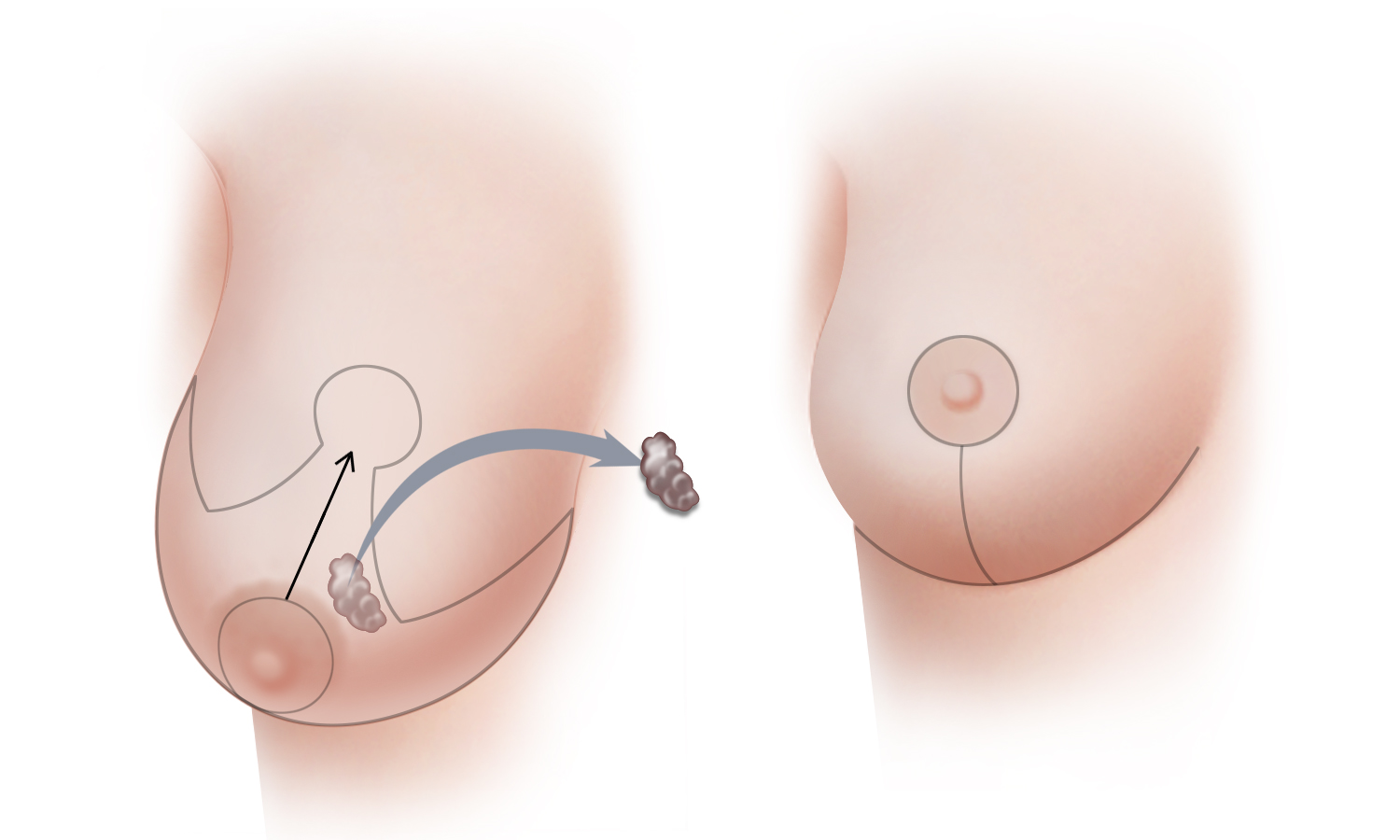
(A) When a lumpectomy or partial mastectomy might distort a woman’s breast, remaining disease-free breast tissue can be sculpted to avoid distortion, realign the nipple and areola, and give the breast a natural appearance. Using oncoplastic techniques to move the remaining breast tissue and fill in defects created by lumpectomy or partial mastectomy, in a manner similar to what is done during a breast reduction or breast lift, breast shape can be better preserved, and in some cases, even enhanced. In addition, a breast lift or breast reduction is frequently performed on the opposite breast to produce symmetry. (B) The scar needed to produce the optimal result will vary from one situation to the next, but frequently the resultant scar is similar to that which results following breast reduction surgery.
(A) When a lumpectomy or partial mastectomy might distort a woman’s breast, remaining disease-free breast tissue can be sculpted to avoid distortion, realign the nipple and areola, and give the breast a natural appearance. Using oncoplastic techniques to move the remaining breast tissue and fill in defects created by lumpectomy or partial mastectomy, in a manner similar to what is done during a breast reduction or breast lift, breast shape can be better preserved, and in some cases, even enhanced. In addition, a breast lift or breast reduction is frequently performed on the opposite breast to produce symmetry. (B) The scar needed to produce the optimal result will vary from one situation to the next, but frequently the resultant scar is similar to that which results following breast reduction surgery.
Oncoplastic surgery can improve the final shape of the breast after breast-conserving surgery without compromising cancer care. When a lumpectomy or partial mastectomy will or might distort a woman’s breast, the remaining tissue can be sculpted to realign the nipple and areola and give the breast a natural appearance. By rotating breast tissue to fill defects created by the lumpectomy or partial mastectomy (in a manner similar to what is done during a breast reduction or breast lift) breast shape can be better preserved. In addition, the opposing breast can also be modified, for example with a breast reduction or breast lift, to improve symmetry. These procedures are usually done on an outpatient basis.
Because surgery is completed prior to radiation, wound-healing problems that occur with significant frequency with post-radiation surgery are minimized, and only a single surgery is necessary.
If you think you may benefit from oncoplastic breast surgery, consultation ahead of lumpectomy surgery is suggested.
Partial Breast Reconstruction in Connecticut and New York
Over time, breast surgery for breast cancer has evolved from severely deforming surgical procedures toward less and less disfiguring procedures and consequently improved cosmetic results. Oncoplastic surgery is not for everyone or every tumor - oncoplastic surgery is only appropriate for carefully selected patients. Breast size, tumor size and location,the ability of the surgeon to remove the tumor with adequate margins, and a woman’s goals and expectations are all factors that collectively determine whether or not oncoplastic surgery is a good option. In the event that breast conservation is not an option or not desirable, state-of-the-art methods of natural-tissue reconstruction after mastectomy may be an excellent option.
Contact us if you would like to make an appointment and learn more about your options for breast conservation and oncoplastic surgery.
Staging of Breast Cancer

Breast Cancer Staging
If a diagnosis of breast cancer is made, more tests will be done to better understand and characterize the cancer and to see if it has spread to other parts of the body. Finding out what stage the cancer has reached—“staging” it—determines which of several treatment options will likely be the most effective. Staging tests include some or all of the following: chest X-ray, ultrasound, bone scan, MRI, CT scan, and PET scan.
The stage of a breast cancer is based on the results of these tests as well as the evaluation breast tissue and lymph nodes removed at surgery, whether as a lumpectomy or as a mastectomy.
The American Joint Committee on Cancer (AJCC) staging system classifies cancers based on T, N, and M status,
- T - Tumor size, and involvement of nearby organs
- N - lymph Node involvement
- M - Metastasis - whether the cancer has spread to distant organs
After the T, N, and M categories are determined, the information is combined to determine the stage. Stage is expressed in Roman numerals from least advanced disease - stage I - to the most advanced disease – stage IV. Of breast cancers, lobular carcinoma in-situ and ductal carcinoma in-situ are considered pre-invasive cancers and are classified as stage 0.
A detailed description of the AJCC staging system is available on the American Cancer Society’s website.
Breast Cancer Symptoms

Symptoms of Breast Cancer
How would I know if I have breast cancer?
Like many types of cancer, breast cancer does not always cause symptoms. In fact, in its earliest stages, breast cancer usually does not cause any symptoms. For this reason, screening tests such as mammograms are used to look for cancer and for precancerous cells even before they cause symptoms or can be felt by you or your doctor.
What are the symptoms of breast cancer?
While breast cancer usually does not cause symptoms at its earliest stage, as a tumor grows, it can change how a woman’s breast looks or feels.
Often, the first subjective sign of breast cancer is a lump in the breast that feels different from the surrounding breast tissue. A woman—or her partner—may discover such a lump accidentally.
Signs and symptoms of breast cancer include:
- A lump in the breast
- Swelling of the breast
- Unusual breast or nipple pain
- Persistent breast pain
- A change in breast size or shape
- Skin dimpling
- Redness or persistent rash of the breast skin, areola or nipple
- Nipple inversion
- Spontaneous nipple discharge
- Lump or lumps in the armpit or collar-bone areas
Many benign breast disorders such as fibroadenomas, fibrocystic change and mastitis are also common causes of many of these symptoms. ANY new breast symptom or finding should be brought to the attention of your doctor immediately as early detection and treatment can significantly improve the chance of a cure in the event that breast cancer is diagnosed.
Breast Reduction

BREAST REDUCTION
Breast reduction surgery (known technically as reduction mammaplasty) removes excess breast tissue to reduce breast size and to contour breast shape. Women with large breasts frequently find that they have physical discomfort from the weight of their breasts, and that as a result they even alter their physical activity and avoid exercise. Improper posture, back and neck pain, indentations from bra straps and skin rashes are commonly the result of having disproportionately large breasts. Breast reduction surgery is usually done to provide physical relief from these symptoms and to achieve a breast size in better proportion to the rest of the body. Breast reduction surgery is also done to improve symmetry between a woman’s breasts, or to achieve symmetry between a reconstructed breast and the breast on the opposite side.
Although relief of symptoms is one goal of breast reduction surgery, producing natural-looking and aesthetically pleasing breasts is also of paramount importance. Breast reduction surgery is usually performed under general anesthesia. Most women are able to return to work within about a week of surgery, unless heavy lifting or strenuous physical activity is involved. More vigorous activity and exercise can usually be resumed in about 3 to 4 weeks.
Breast Reduction Type A
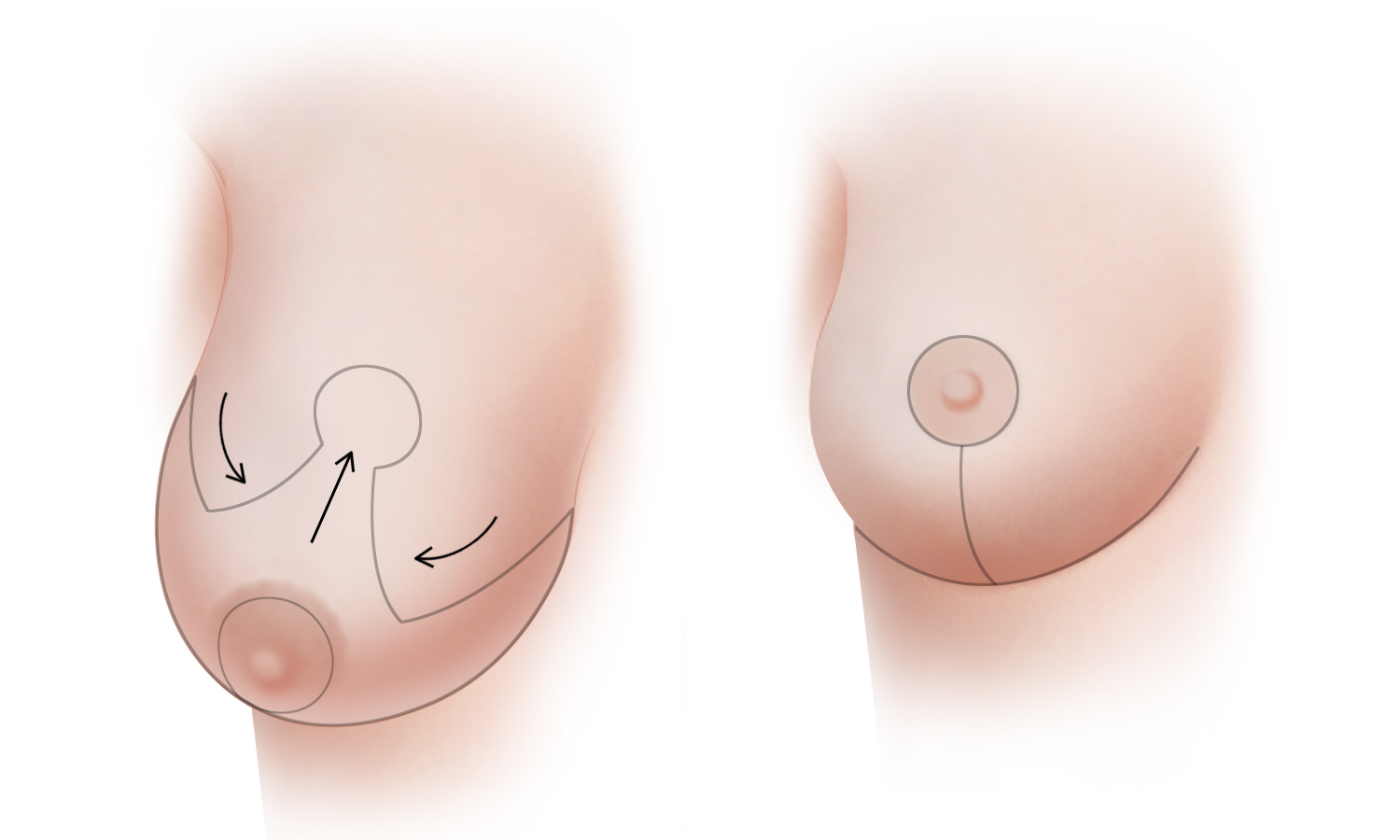
Breast reduction surgery (known technically as reduction mammaplasty) removes excess breast tissue, and skin to reduce breast size and to contour the shape of the breasts. (A) The “anchor-pattern” scar, also known as a Wise-pattern scar (named after the surgeon who initially described this approach to breast reduction) typically allows for the greatest reduction in breast size and also facilitates reshaping of significantly droopy breasts. The use of an anchor-pattern scar is often required when large breasts are reduced
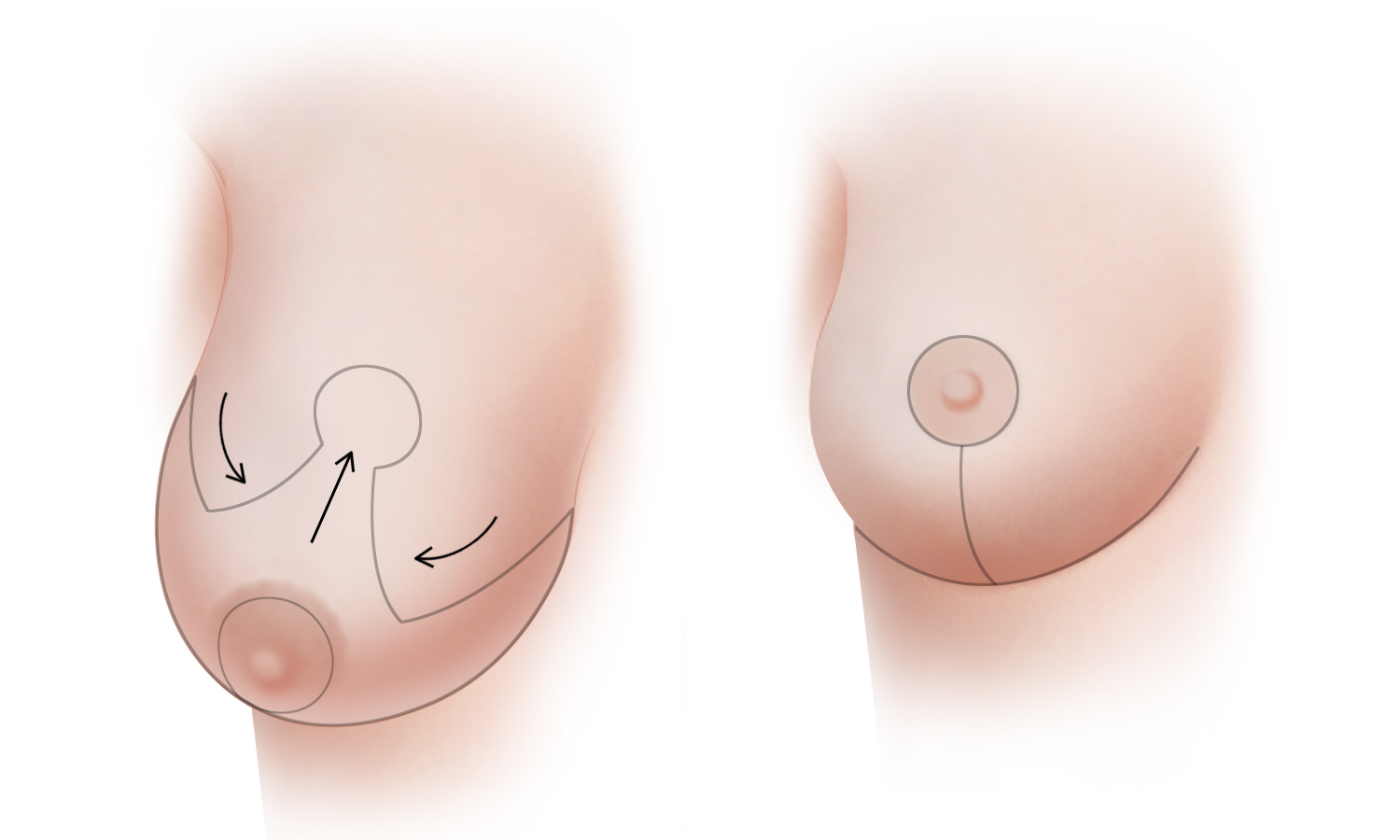
Breast reduction surgery (known technically as reduction mammaplasty) removes excess breast tissue, and skin to reduce breast size and to contour the shape of the breasts. (A) The “anchor-pattern” scar, also known as a Wise-pattern scar (named after the surgeon who initially described this approach to breast reduction) typically allows for the greatest reduction in breast size and also facilitates reshaping of significantly droopy breasts. The use of an anchor-pattern scar is often required when large breasts are reduced
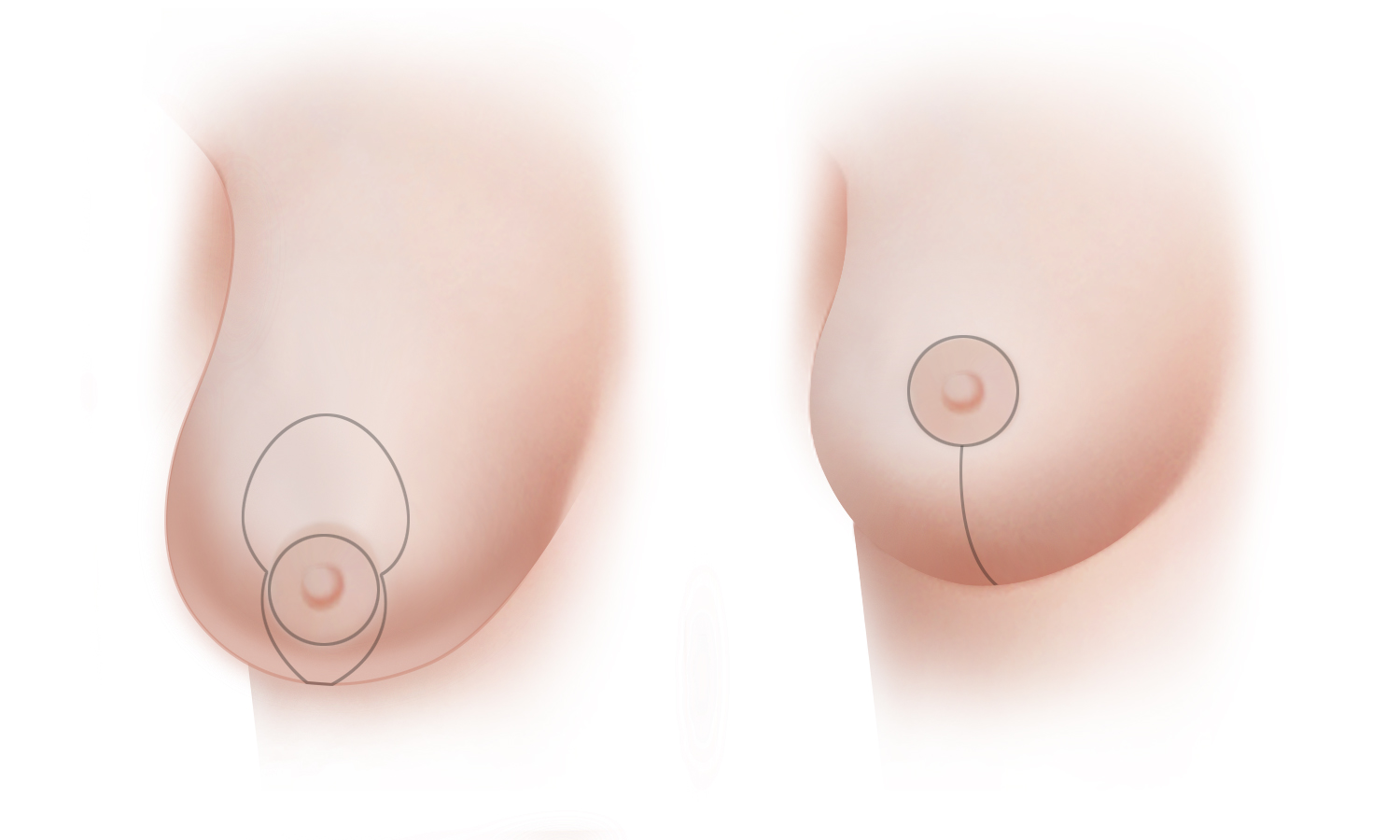
(B) The “vertical” or “lollipop” breast reduction technique, like the anchor-pattern technique, produces a scar around the areola as well as vertically along the lower central portion of the breast, however, with this approach, a scar in the lower breast crease is avoided. This approach is generally optimal for patients with moderate sized breasts who desire a decrease in overall breast volume.
Breast Reduction Type B
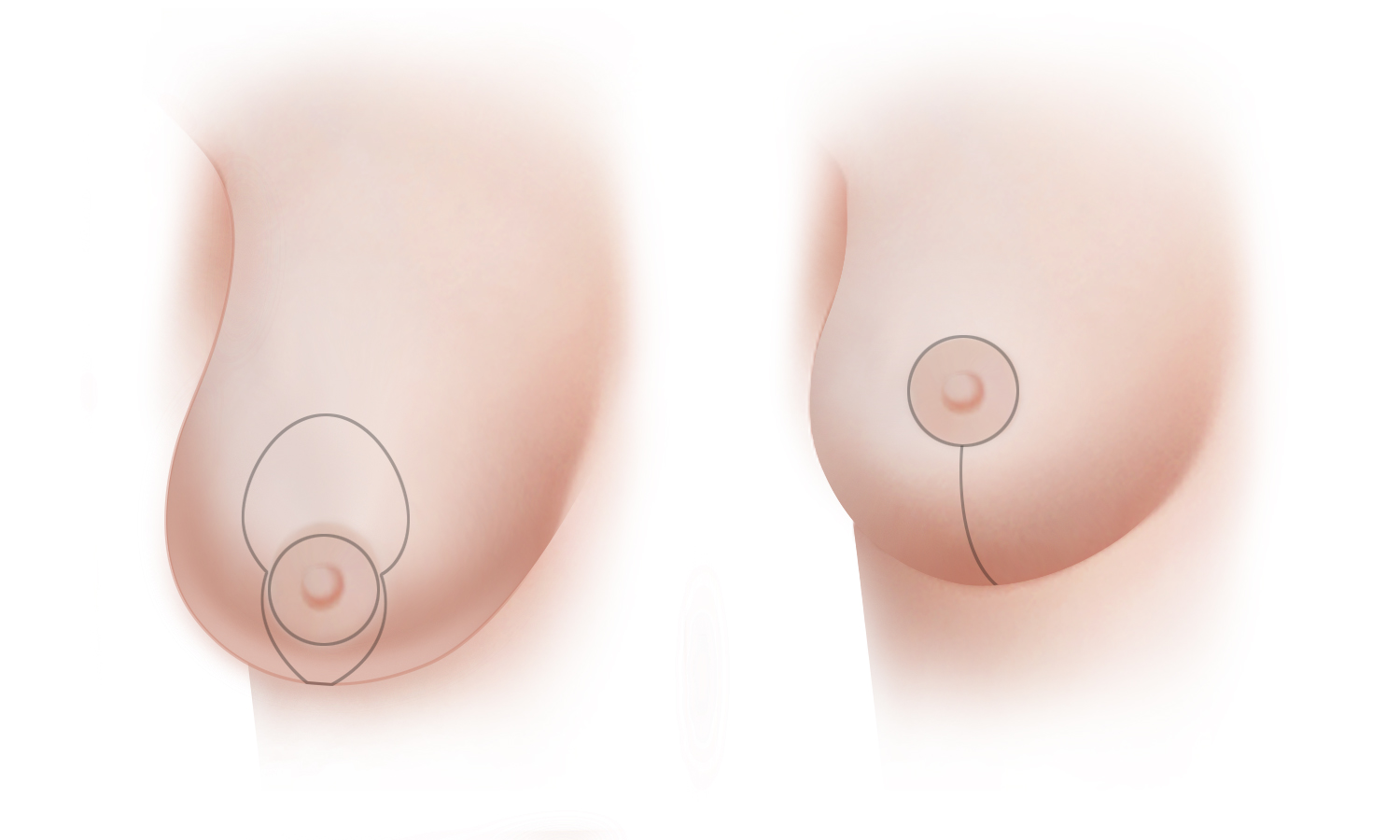
(B) The “vertical” or “lollipop” breast reduction technique, like the anchor-pattern technique, produces a scar around the areola as well as vertically along the lower central portion of the breast, however, with this approach, a scar in the lower breast crease is avoided. This approach is generally optimal for patients with moderate sized breasts who desire a decrease in overall breast volume.
Breast Lift

BREAST LIFT
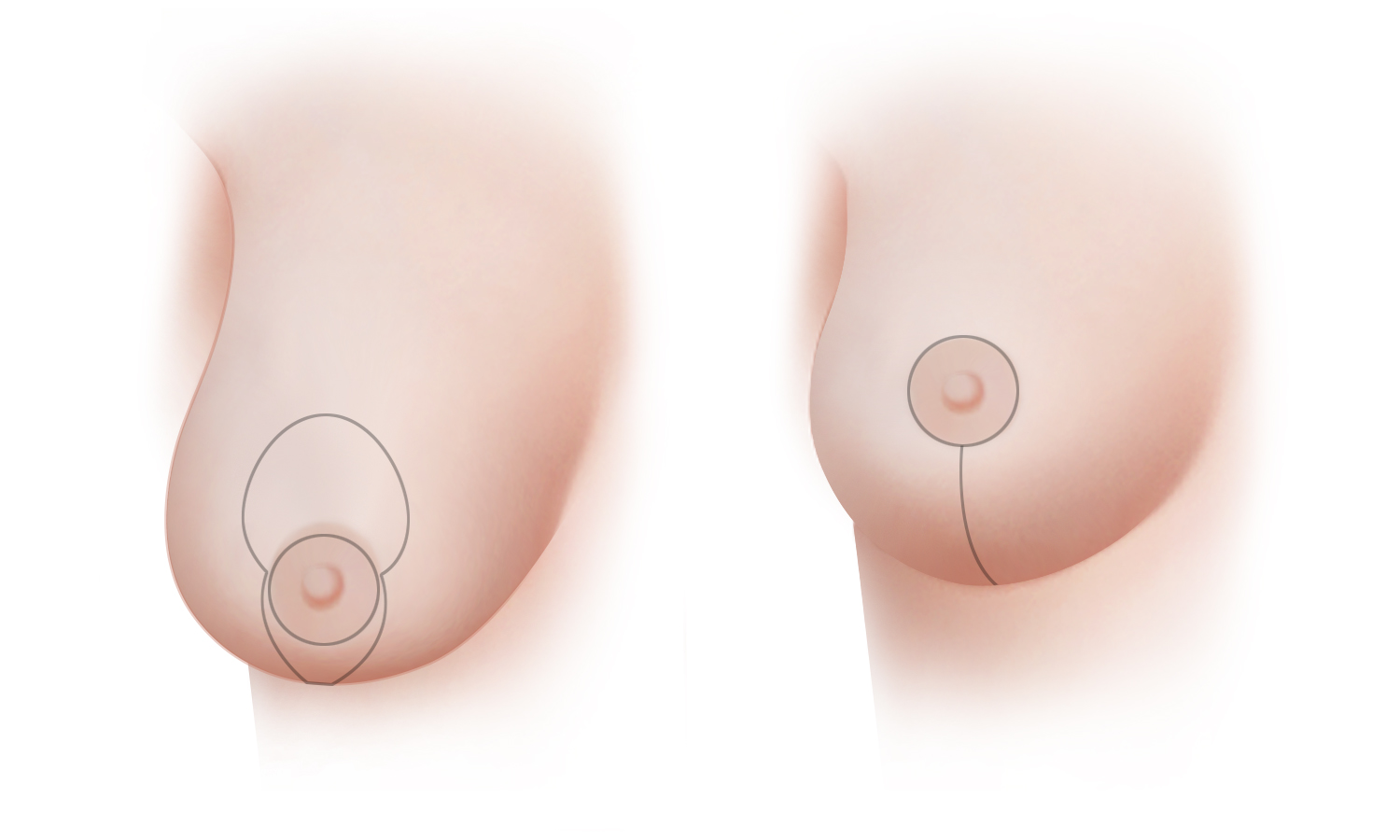
A breast lift, or mastopexy, can restore a more youthful shape and a firmer feel to the breasts. (A) Excess skin is removed and the breast tissue is surgically sculpted to support the new contour of the breast. In addition to raising and firming the breast, the nipple and areola are lifted to a higher position. (B) The scar for a mastopexy can occasionally be limited to the perimeter around the areola, but most often, a breast lift includes a vertical scar from the bottom of the areola to the crease that defines the bottom of the breast (known technically as the inframammary fold).
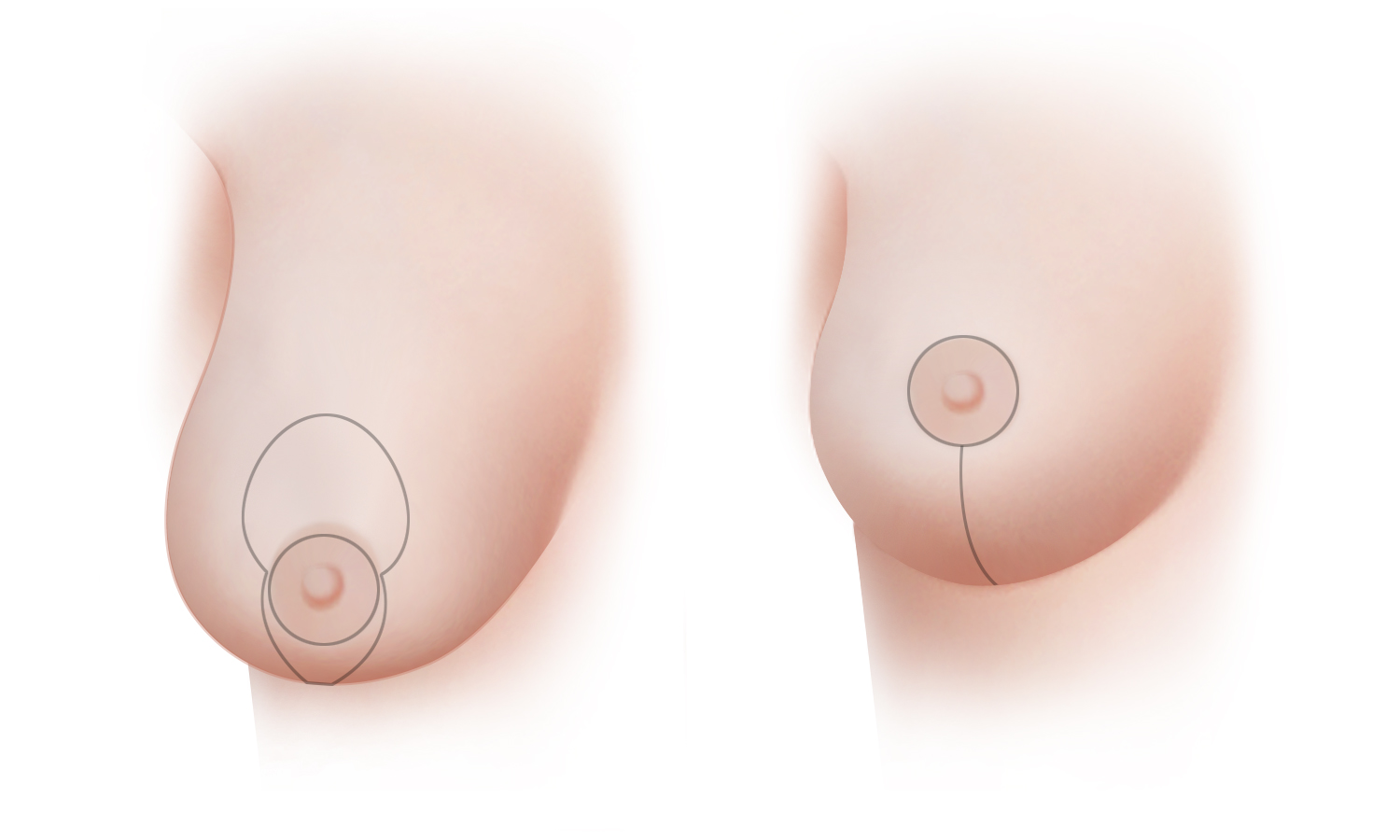
A breast lift, or mastopexy, can restore a more youthful shape and a firmer feel to the breasts. (A) Excess skin is removed and the breast tissue is surgically sculpted to support the new contour of the breast. In addition to raising and firming the breast, the nipple and areola are lifted to a higher position. (B) The scar for a mastopexy can occasionally be limited to the perimeter around the areola, but most often, a breast lift includes a vertical scar from the bottom of the areola to the crease that defines the bottom of the breast (known technically as the inframammary fold).
Excess skin is removed and the breast tissue is surgically sculpted to support the new contour of the breast. In addition raising and firming the breast the nipple and areola are lifted to a higher position. Whenever possible, Dr. Greenspun uses a minimal-incision vertical technique to reshape and lift the breasts, a technique which produces a minimal amount of scarring. A breast lift can be performed under general anesthesia or under local anesthesia in combination with sedation.
Most women are able to return to work within about a week of surgery, unless heavy lifting or strenuous physical activity is involved. More vigorous activity and exercise can usually be resumed in about 3 to 4 weeks.
Breast Lift Surgery in New York and Connecticut
Contact us if you would like more information about breast lift procedures or to schedule a consultation. Our practice has offices in New York City and Greenwich, Connecticut.
Prophylactic Mastectomy

Prophylactic Mastectomy and Breast Reconstruction
Some women find significant peace of mind in having preventative surgery, because their risk of developing cancer is considerable. Prophylactic mastectomy is surgery to remove one or both breasts in order to reduce the risk of developing breast cancer in the future. The need for frequent surveillance, numerous biopsies, and the fear of developing cancer can be reduced, if not eliminated, with prophylactic mastectomy.
When combined with immediate reconstruction, a woman having, prophylactic mastectomies can wake up from the surgery with reconstructed breasts. When nipple-sparing or skin-sparing mastectomy are combined with autologous tissue reconstruction, the newly reconstructed breasts will be as realistic and natural-looking as possible.
Women considering prophylactic mastectomy are likely to:
- Have a strong family history of breast cancer
- Have a personal history of breast cancer or at present have breast cancer in one breast
- Have tested positive for BRCA1 or BRCA2 gene mutations
- Have been diagnosed with lobular carcinoma in situ (LCIS)
- Have had radiation therapy to the chest before age 30
- Have widely spread breast microcalcifications or have dense breasts; both of these factors make breast cancer screening more challenging.
If you are or may be at high risk for developing breast cancer, it’s important to discuss all your options for risk reduction and surveillance with your doctors. Prophylactic mastectomy can reduce the risk of developing breast cancer roughly 90 to 95 percent. Nevertheless, making a decision about whether or not to undergo this procedure will obviously be considered very carefully. The availability of high quality breast reconstruction may help make your decision about a prophylactic mastectomy easier.
Contact us if you would like to make an appointment to discuss breast reconstruction after mastectomy.
Lumpectomy

LUMPECTOMY
Lumpectomy, also called a partial mastectomy, segmental mastectomy or quardantectomy, is the surgical removal of a breast tumor along with some of the normal breast tissue that surrounds it. Multicenter clinical trials have demonstrated that in certain early stages of breast cancer, lumpectomy, when combined with postoperative radiation therapy, can produce long-term survival rates on par with mastectomy without radiation.
Depending on the breast size and shape, the amount of tissue removed to treat the cancer, and the changes that can occur in breast shape after radiation, breast-sparing procedures can leave the breast’s contours such that there may be no need for further reconstruction. In other situations, however, the aesthetic results of breast-conserving surgery may be disappointing.
- Standard breast-conserving therapy, unfortunately, has its limits and has been shown to yield poor cosmetic results up to 30 percent of the time
- Some women may find that the shape of their breast treated with breast conserving surgery becomes distorted after radiation therapy is completed
In spite of the potential aesthetic shortcomings, for many women, the ability to save a part of their breast makes the option of breast conserving therapy very appealing. When a breast conserving procedure such as lumpectomy will or might distort the shape of a woman’s breast, a plastic surgeon can work together with a breast oncologic surgeon at the time of surgery, to help best preserve or restore the shape of your breast. Oncoplastic surgery combines innovative plastic surgery techniques with breast surgical oncology to maximize both the oncologic outcomes and cosmetic results of breast conserving surgery.
In the event that the results of breast-conserving surgery are disappointing, delayed breast reconstruction may be able to improve the appearance of the breast and restore a more natural shape.
Breast Implant Lifespan

Breast Implant Lifespan
While there are many women who are happy and satisfied with their implant-based breast reconstructions, we think it is important that women considering breast implants understand certain significant information. Perhaps most importantly, a high rate of unplanned re-operation has repeatedly been demonstrated for women who opt to have an implant-based breast reconstruction.
According to the Food and Drug Administration (FDA), the agency responsible for regulating breast implants, common consequences of implant reconstruction include unplanned re-operation and implant failure. It is also important to know that routine MRI (every two years beginning three years after surgery) is recommended for women who have silicone-filled breast implants to monitor for rupture.
A common myth suggests that women who have breast implants breast need to have their implants changed every ten years. While there is no need to routinely remove and replace breast implants regardless of how long they have been in a person’s body, problems with implants that require additional surgery including implant removal, occur increasingly the longer an implant has been in place. FDA makes clear that breast implants are not lifetime devices.
The Bottom Line According to the FDA
The risks and benefits of surgery involving a breast implant should be carefully weighed.
The information below comes directly from the FDA’s website:
- Breast implants are not lifetime devices; the longer you have your implants, the more likely it will be for you to have them removed
- The longer you have breast implants, the more likely you are to experience local complications and adverse outcomes
- The most common local complications and adverse outcomes are capsular contracture, re-operation, and implant removal. Other complications include rupture or deflation, wrinkling, asymmetry, scarring, pain, and infection at the incision site
- You should assume that you will need to have additional surgeries (re-operations)
- Many of the changes to your breast following implantation may be cosmetically undesirable and irreversible
Date collected by FDA and published in the official labeling of breast implants find that:
- Approximately 40% of women will require unplanned re-operation within 5 years
- Approximately 50% of women will require unplanned re-operation within 7 years
- Roughly 1 of 3 women who have an unplanned re-operation will require at least one more additional unplanned re-operation within 3 years
- One or more times over the course of a patient’s life, she will require surgery to have her implants removed because of rupture or other complications
- If radiation has been, or will be, part of a woman’s breast cancer treatment, there is an even higher rate of complications associated with the use of implants
Fat Grafting

Fat Grafting and Fat Injection for Breast Reconstruction
Fat grafting (or as it is also known, fat transfer, fat injection or lipoinjection) has long been used by plastic surgeons to smooth sunken areas on the face and to add fullness to the cheeks and lips. Fat grafting can also be used to refine the results of breast reconstruction surgery. This technique can be used to:
- Add volume to a breast reconstructed with natural tissue
- Smooth areas that have an irregular contour or are depressed, or to better sculpt the shape of a reconstructed breast
- Camouflage an implant used for reconstruction
- Help restore a more natural transition between the upper chest and a reconstructed breast.
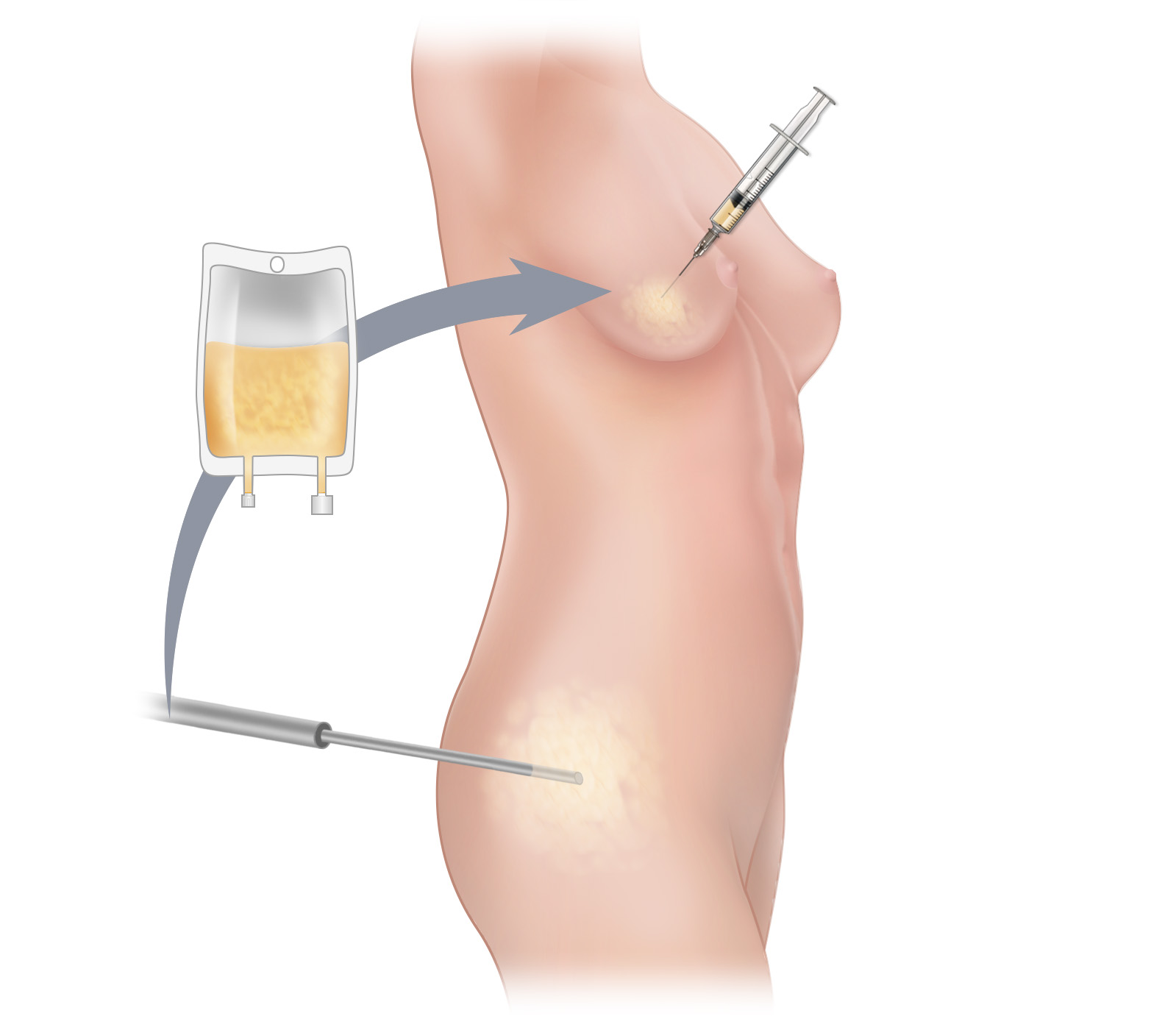
Fat grafting is an outpatient surgical procedure that moves fat from one part of the body to another. In breast reconstruction, this technique is commonly used to make subtle adjustments to the shape and contour of a breast reconstructed with either natural tissue or a breast implant. Fat grafting can sometimes also be used to increase the size of a breast reconstructed with a woman’s own tissue. The fat used for grafting is obtained by means of a gentle liposuction-like approach, after which the fat cells are purified and injected into the desired area. Only very tiny incisions are necessary, and as a result, scarring is minimized and often almost undetectable. Furthermore, since fat is obtained from areas where it is unwanted, many people experience enhanced appearance at the donor site following fat grafting. When fat grafting is used to smooth the contours of a breast reconstructed with an implant, keep in mind that excess fat may be used up in the grafting process and preclude the possibility of future natural-tissue flap surgery.
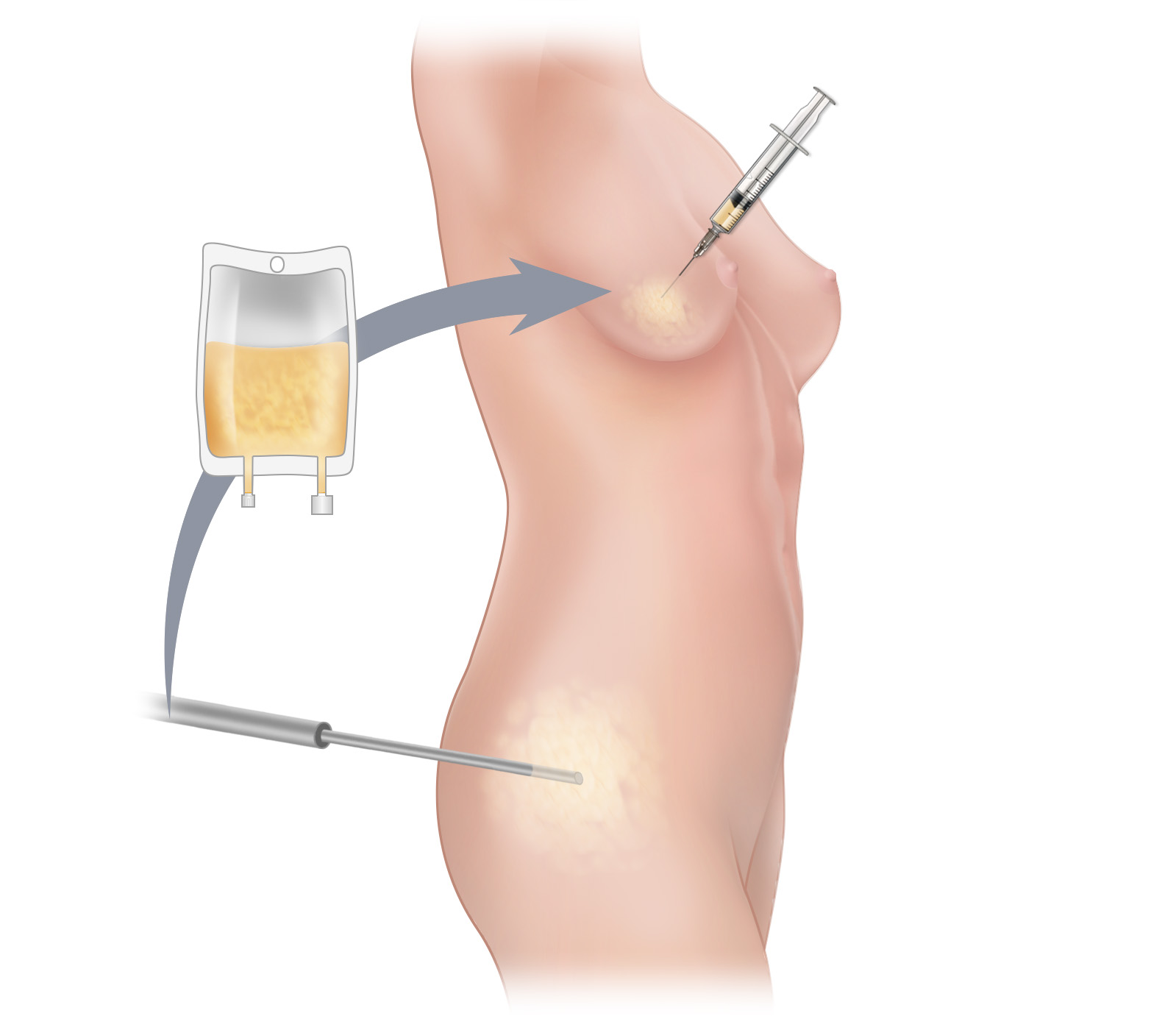
Fat grafting is an outpatient surgical procedure that moves fat from one part of the body to another. In breast reconstruction, this technique is commonly used to make subtle adjustments to the shape and contour of a breast reconstructed with either natural tissue or a breast implant. Fat grafting can sometimes also be used to increase the size of a breast reconstructed with a woman’s own tissue. The fat used for grafting is obtained by means of a gentle liposuction-like approach, after which the fat cells are purified and injected into the desired area. Only very tiny incisions are necessary, and as a result, scarring is minimized and often almost undetectable. Furthermore, since fat is obtained from areas where it is unwanted, many people experience enhanced appearance at the donor site following fat grafting. When fat grafting is used to smooth the contours of a breast reconstructed with an implant, keep in mind that excess fat may be used up in the grafting process and preclude the possibility of future natural-tissue flap surgery.
Recovery time is minimal, and most women can return to work and/or other non-strenuous activities the day after the procedure. Vigorous or strenuous activity and exercise can be resumed approximately two weeks after fat transfer. When performed for reconstructive purposes, your medicalinsurance coverage will generally cover this treatment.
Fat Grafting for Breast Reconstruction in New York and Connecticut
Contact us if you would like more information about the options for micro-fat injection for breast reconstruction or to schedule a consultation. Our practice has offices in New York City and Greenwich, Connecticut.
Breast Augmentation

BREAST AUGMENTATION
Breast augmentation is one of the most frequently performed cosmetic surgery procedures. Women elect to undergo breast augmentation for many different reasons: to balance breast size, to compensate for reduced breast volume that frequently occurs following pregnancy or with increasing age, or simply to change the size and appearance of their breasts.
Breast Augmentation with Implants
By placing either saline- or silicone-filled implants beneath the existing breast tissue or below the chest wall muscle, augmentation can give a woman larger and firmer breasts. Although most patients who have breast augmentation are pleased and satisfied with the results, every woman considering this surgery should be well aware of the following information about breast implants:
Implant lifespan
Breast implants, like other medical devices, are not expected to last indefinitely. They are not considered lifetime devices, and any woman who has implants placed should know that, at some point in her life, she will likely need surgery to replace the implants.
Need for further surgery
Studies done by the Food and Drug Administration (FDA) suggest that most women with implants will most likely need to have further surgery at some point during their lives, for one or more of these reasons: implant rupture, capsular contracture (hardening of the implant), a shift in the implants position, or a change in breast shape or volume. Additional information about breast implants is available on the FDA website.
Mammography and MRI
Women with breast implants need to have their mammograms performed at centers that use special displacement techniques, which require more views and possibly additional exposure to radiation. Mammography may not be as sensitive in women with implants, although women with implants are not shown to have any increased risk of breast cancer. When the FDA approved silicone implants for cosmetic breast augmentation in 2006, they determined that women with silicone gel breast implants should have a breast MRI three years after getting silicone implants and every two years after that. The purpose of these MRIs is to determine if the silicone gel breast implants are ruptured or leaking, because often leaks and ruptures have no symptoms. It is important to remove silicone implants if they are ruptured, to avoid having the silicone leak into the breast or lymph nodes. Many insurance plans do not cover the cost of these MRI tests, which can cost $2,000 or more.
Insurance
Health insurance premiums may increase for women with breast implants and treatment of complications related to breast implants may not be covered.
Additional information about breast implants and health insurance coverage is available at WebMD.
Breast Augmentation Using Your Own Tissue
Some women may wish to undergo breast enhancement without the use of a synthetic implant. In this case, perforator flaps may be an attractive option. Although much more commonly used for breast reconstruction following mastectomy, perforator flaps can be used to add volume to a woman’s breasts with her own body’s tissue. Furthermore, for women who are experiencing implant-related complications following breast augmentation, perforator flaps can potentially be used to replace synthetic breast implants with soft natural tissue. Similarly, these procedures may be an appealing option for women who no longer want to have their breast implants, but who still wish to maintain the larger breast size implants offer.
When your own tissue is used for breast augmentation (known technically as autologous augmentation), it is yours for life, and problems related to the use of implants (for example, capsular contracture, leak and rupture) are eliminated.
Breast Augmentation in New York and Connecticut
Contact us if you would like more information about breast augmentation or breast enhancement surgery or to schedule a consultation. Our practice has offices in New York City and Greenwich, Connecticut.
Breast Implants

Breast Reconstruction with Breast Implants
Reconstruction with breast implants involves restoring the form of the breast by inserting, into the mastectomy site, a breast prosthesis made of synthetic material. Implants come in a variety of shapes and sizes; they have an outer shell made from silicone that is filled with either saline or silicone gel. Although there has been considerable concern over the safety of silicone-gel filled implants, their use is currently approved by the U.S. FDA.
While implant reconstructions generally require the shortest initial hospitalization of all the possible methods of breast reconstruction—and some women find implant reconstructions appealing for this and other reasons—many patients and many doctors are troubled by the high rate of unplanned re-operation associated with this method of reconstruction. Unfortunately, common consequences of implant reconstruction include re-operation and the need to remove implants, according to the U.S. Food and Drug Administration. Large studies of women who had breast reconstruction using implants have found that:
- Approximately 40% of women will require unplanned re-operation within 5 years, and approximately 50% will require unplanned reoperation within 7 years
- One or more times over the course of the patient’s life, she will probably need to have her implants removed because of rupture or other complications
Complications & Limitations
Some of the more frequently occurring complications that can lead to the need for additional surgery and possibly implant removal include:
- Capsular contracture
- Leak or rupture
- Rippling or wrinkling
- Infection
- Extrusion or exposure of the implant through the skin
- Shifting or migration of an implant to an undesirable position
The FDA publication Breast Implants––Potential Local Complications and Reoperations provides a more through review.
If radiation has been or will be part of the treatment of a woman’s breast, there is an even higher rate of complications associated with the use of implants, and aesthetic results may be adversely affected.
For women contemplating reconstruction of just one breast, an additional consideration may be the degree to which a breast reconstructed with an implant will be able to match the uninvolved breast, in both appearance and feel.
Advantages to Breast Implant Reconstruction
In spite of the drawbacks and complications unique to implants, there are some advantages to implant breast reconstruction as compared to natural tissue breast reconstruction. That this method of reconstruction typically requires the shortest period of hospitalization of all methods of reconstruction may be appealing to some women. Because there is no “donor site”, there is no additional scar elsewhere on the body and no need to heal at a site other than the breast. Additionally, some women who have medical conditions that could compromise the safety of reconstructive surgery using their body’s own tissue may be able to undergo implant reconstruction safely.
The advantages of this quicker and technically less demanding reconstruction method should be weighed against the disadvantages of later complications, including capsular contracture and a high rate of unplanned re-operation and the lifespan of breast implants.
Breast Reconstruction Without Breast Implants
For women who wish to undergo restorative breast surgery without an implant, natural-tissue reconstructive procedures may be appealing.
Related Breast Reconstruction Procedures

Breast Reconstruction - Associated Procedures
Some women may choose to undergo surgical breast procedures, unrelated to mastectomy, for other medical or cosmetic reasons. Some of these same procedures procedures are also used for women who undergo post-mastectomy reconstruction—for example to create a more balanced overall look by altering the unaffected breast when just one breast is reconstructed.
Nipple Reconstruction
Regardless of which method of breast reconstruction you may choose, reconstruction of a nipple—a minor surgical procedure—really helps to make a reconstructed breast look as natural as possible.
Fat Grafting
Fat grafting, also known as lipofilling, can be used in many ways to refine the results of breast reconstruction surgery. For example, the technique can be used to add volume to a breast reconstructed with natural tissue, to smooth areas that have an irregular contour, or to camouflage the edges of an implant used for reconstruction.
Breast Reduction
Breast reduction surgery removes excess breast tissue to reduce breast size and, at the same time, lifts and contours the breasts to produce natural-looking and aesthetically pleasing breasts.
Breast Lift
A breast lift can restore a more youthful shape and a firmer feel to the breasts; this procedure can be done for purely cosmetic reasons, to improve symmetry between a woman’s breasts, or to achieve symmetry between a reconstructed breast and the opposite breast.
Breast Augmentation
Breast augmentation, one of the most frequently performed cosmetic surgery procedures, can be done to change the size and appearance of a woman’s breasts, balance breast size, or compensate for the reduced breast volume that frequently occurs following pregnancy or from aging.
Lymphedema Surgery
Some women treated for breast cancer develop arm, breast, and chest swelling called lymphedema. The treatment of lymphedema involves many different modalities, including surgery. Sometimes, surgery makes it possible to reduce the swelling of lymphedema and significantly improve a person’s quality of life.
Tubular Breast Correction
One of the most common abnormalities of breast shape is known as a tubular breast or tuberous breast. Breast implants or natural tissue can be used to correct tubular breasts and create a more aesthetically desirable appearance.
Botched Breast Reconstruction Repair
Corrective breast reconstruction can be an excellent option if you are unhappy with your breast reconstruction, feel that your breast reconstruction may have been done inadequately, or have had a breast reconstruction failure.
Surgery

Surgery for Breast Cancer
Most women who are diagnosed with breast cancer will undergo some form of surgery to remove the cancer from their breast. In addition, most women with breast cancer will also have one or more of the lymph nodes under the armpit removed and evaluated, often using a technique called sentinel lymph node biopsy, to see if cancer cells have spread there.
The surgical procedures used to treat breast cancer remove either part or all of the breast tissue. Procedures that remove only a portion of the breast tissue are called breast-conserving or breast-sparing; removal of all of the breast tissue is called a mastectomy.
Breast-Conserving Surgery
Breast-conserving procedures remove the cancer along with a portion of the breast tissue. These procedures traditionally include:
When a lumpectomy or partial mastectomy may distort the appearance of a woman’s breast, oncoplastic surgery may be an option. Oncoplastic surgery is a relatively new surgical option for women who desire breast conservation; this approach combines breast surgical oncology with plastic surgical reconstruction in a single procedure.
- Oncoplastic Surgery
- Radical mastectomy
- Modified radical mastectomy
- Simple mastectomy
- Skin-sparing mastectomy*
- Nipple-sparing mastectomy*
Mastectomy
Mastectomy removes all of the breast tissue and variable amounts of other nearby tissue. These procedures include:
(* all or most of the skin overlying the breast is preserved with these types of mastectomies)
Because the skin that covers the breast tissue is not actually part of the breast gland, it is almost never necessary to remove large amounts of skin when treating breast cancer. When combined with breast reconstruction, preservation of a maximal amount of skin with a skin-sparing or nipple-sparing mastectomy will generally result in the best possible aesthetic results.
Chemotherapy

Chemotherapy for Breast Cancer
Chemotherapy is a cancer treatment that uses medication to slow or stop the growth of cancer cells. Chemotherapy drugs either kill cancer cells or stop them from dividing. Since some normal cells involved in the healing or surgical wounds are also affected by chemotherapy, your breast management team will also take into account whether or not chemotherapy will be part of your treatment when planning your reconstruction.
In general, the need for a woman to receive chemotherapy does not preclude immediate breast reconstruction. If neo-adjuvant (before surgery) chemotherapy is administered, mastectomy, with or without reconstruction will generally follow a woman’s last dose by four to six weeks. During the weeks between chemotherapy and surgery, your immune system will have time to recuperate so that it will be prepared to help you heal after surgery. When adjuvant (after surgery) chemotherapy is part of a woman’s treatment, it usually begins about six weeks after mastectomy or mastectomy with reconstruction in order to give the body time to heal. In rare cases, wound healing problems following reconstruction could delay the initiation of chemotherapy. Nevertheless, well controlled studies have shown that immediate breast reconstruction is considered safe for the overwhelming majority of women even when chemotherapy is planned after mastectomy. This is because breast reconstruction does not generally delay the start of chemotherapy.
» Contact us if you would like to make an appointment and learn more about your options
Hormone Therapy

Hormone Therapy for Breast Cancer
Hormones are circulating substances produced by different glands of the body, and they can cause some breast cancers to grow. If tests show that a woman’s cancer is sensitive to the action of hormones, she may benefit from treatments that reduce their effect. Tamoxifen®, for example, is a medication that blocks the effects of the hormone estrogen and is commonly used in the treatment of breast cancer. Arimidex® is another commonly used hormonal therapy for breast cancer. Your breast surgeon and oncologist will determine if hormone therapy may be effective. In most situations, the need for hormone therapy does not affect whether a woman is a candidate for breast reconstruction surgery.
» Contact us if you would like to make an appointment and learn more about your options
Radiation Therapy

Radiation Therapy for Breast Cancer
What Are the Implications of Radiation for Breast Reconstruction?
Radiation may be used in the treatment of some women with breast cancer. A targeted beam of radiation is directed to the chest, and sometimes to the armpit, in order to help rid the body of microscopic tumor cells. Although normal cells are less susceptible to the effects of radiation than the cancer cells, they are not unaffected. Non-cancerous tissues that are in the path of the radiation are changed permanently. In particular, there is a significant loss of skin elasticity that can profoundly affect the aesthetic results of a breast reconstruction in women who are treated with radiation. In addition, there may be more complications when radiation follows reconstructive breast surgery of all types, because the body’s wound-healing mechanisms are altered by exposure to radiation.
Radiation is especially problematic for women who undergo implant reconstructions, regardless of whether the radiation is administered before or after the implant is placed. Some of the complications that occur at higher rates in patients who receive with radiation with implants include wound breakdown, delayed healing, infection, breast implant or tissue expander extrusion, and severe capsular contracture. Natural-tissue reconstruction has the benefit of bringing non-radiated, healthy, well-vascular tissue into the radiated area which can actually aid in the healing process. Because of the potential complications associated with implants, breast reconstruction using natural tissue is generally considered the best method for women who will require or have already had radiation.
The need for radiation to treat the cancer may thus be a factor in determining if a woman will undergo an immediate or delayed breast reconstruction and also in determining which method of reconstruction she chooses.
Timing of Reconstructive Surgery When Radiation Therapy is Necessary
While radiation therapy can complicate breast reconstruction surgery, with proper preparation, most women can achieve a satisfactory reconstruction even if radiation therapy is part of their treatment plan.
Ideally, to achieve the best cosmetic results with the lowest rate of complications, we like to wait approximately six months before performing a perforator flap reconstruction when a woman has had radiation to her breast or chest; this time period may vary depending on a woman’s particular circumstances. Some of the radiation-damaged skin can be replaced with soft and supple skin that allows for the shaping of a much more natural appearing breast. Furthermore, if reconstruction is delayed until after radiation is completed, the tissue used for the reconstruction is not exposed to any radiation that could potentially affect it.
The need for radiation therapy cannot always be determined prior to surgery. This is because evaluation of a mastectomy specimen by a pathologist may uncover certain findings that lead to the determination that radiation is needed to optimally treat a woman’s cancer. Consequently, on occasion, a woman may have already begun the reconstructive process when she learns that she will undergo radiation treatment. Since treatment of the cancer takes precedence, radiation will be administered and if necessary appropriate measures will be taken to optimize the final reconstruction and manage any complications that arise.
» Contact us if you would like to make an appointment and learn more about your options
Mastectomy

Mastectomy and Breast Reconstruction
All mastectomy procedures remove the breast glad. These procedures differ from one another with regard to what other structures are additionally removed and in terms of how much skin remains after the procedure.

Regardless of which of a number of different incisions are used, a mastectomy removes the entire breast gland. While every type of mastectomy may not be right for every patient, the type of incision and the amount of skin removed both affect the aesthetic results of reconstruction. (A) A traditional mastectomy incision takes the shape of an ellipse, and removes the nipple, areola and all of the skin between the two incisions. (B) Skin-sparing mastectomy removes the nipple and areola, but preserves almost all of the remaining breast skin. (C) Nipple-sparing mastectomy, preserves the nipple, areola and breast skin, and thus allows for the most realistic outcomes following reconstruction.

Regardless of which of a number of different incisions are used, a mastectomy removes the entire breast gland. While every type of mastectomy may not be right for every patient, the type of incision used and the amount of skin removed will affect the aesthetic results of reconstruction. (A) A traditional mastectomy incision removes the nipple, areola and all of the skin between the two incisions. (B) Skin-sparing mastectomy removes the nipple and areola, but preserves almost all of the remaining breast skin. (C) Nipple-sparing mastectomy, performed through a single incision, allows total preservation of the nipple, areola and breast skin, and hence the most realistic outcomes following reconstruction.
Radical Mastectomy: removes chest wall muscles in addition to the removal of the breast gland and lymph nodes. This procedure is very rarely performed today.
Modified Radical Mastectomy: like simple mastectomy, removes all of the breast glad and a variable amount of skin. This procedure, however, also removes most or all of the lymph nodes from the armpit and the lining of the chest wall muscles.
Simple Mastectomy: (also known as Total Mastectomy) removes the entire breast gland and a variable amount of the skin of the breast. When done in the “traditional” manner, simple mastectomy removes an ellipse of skin that includes within it, the nipple and areola. In many cases, simple mastectomy will be combined with the removal of one or more of the lymph nodes from the armpit for biopsy.
Skin-Sparing Mastectomy and Nipple-Sparing Mastectomy: These procedures are sophisticated variations of simple mastectomy. They preserve a maximal amount of skin (and in the case of the latter, the nipple and areola) and consequently lend themselves to the best possible reconstructive outcomes especially when combined with immediate breast reconstruction. Learn more about the advantages of combining skin-sparing mastectomy or nipple-sparing mastectomy with immediate breast reconstruction.
» Contact us if you would like to make an appointment to discuss breast reconstruction after mastectomy
» View photographs of the results of breast reconstruction after mastectomy
Skin-Sparing Mastectomy

SKIN-SPARING MASTECTOMY
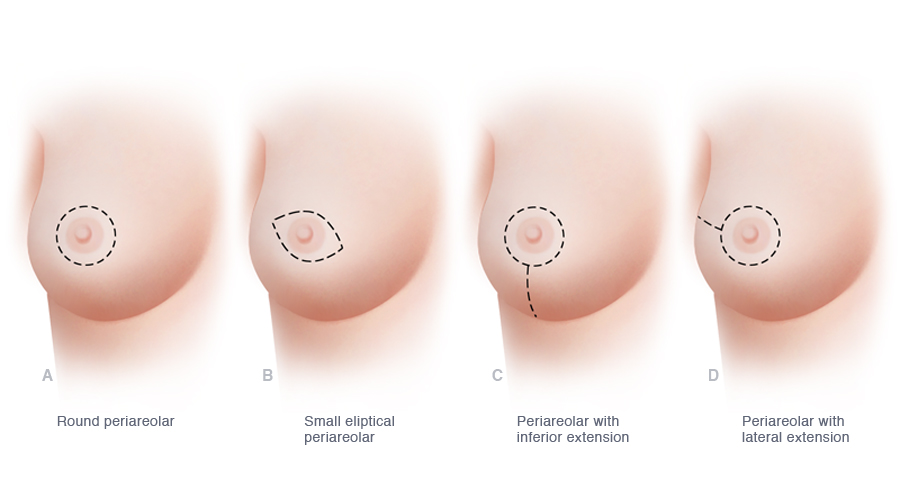
Several possible incisions can be used for skin-sparing mastectomy. Compared to a traditional mastectomy incision, skin-sparing mastectomy removes far less breast skin and thus, when combined with immediate breast reconstruction, helps to optimize the cosmetic results of reconstruction. Several of the more commonly used incisions for skin-sparing mastectomy are illustrated.
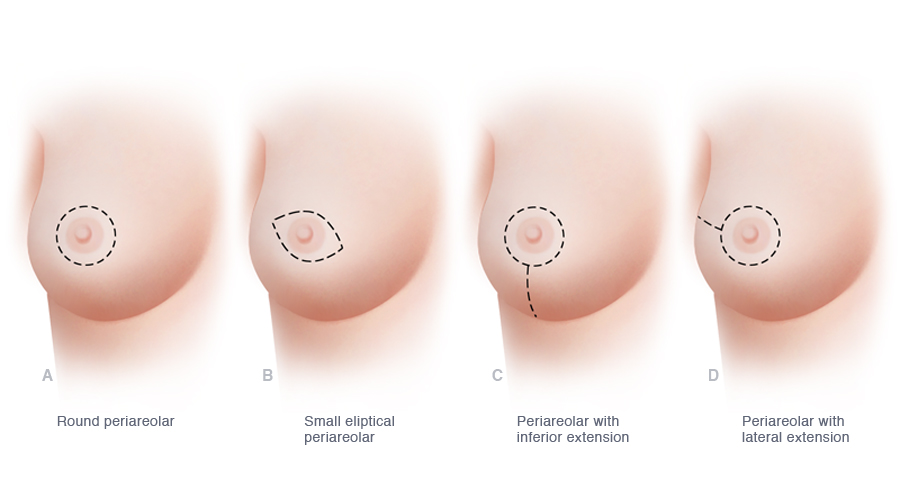
The various possible incisions used when a skin-sparing mastectomy is performed preserve most or all of the skin of the breast but allow for removal of the nipple and areola. Compared to traditional mastectomy, skin-sparing mastectomy, when combined with immediate breast reconstruction, minimizes scarring on the breast and helps optimize the cosmetic results of reconstruction. Several of the more commonly used incisions for skin-sparing mastectomy are illustrated.
Clinical research in the field of breast cancer surgery shows that skin-sparing mastectomy (SSM) maximizes breast skin preservation and significantly improves the symmetry and natural appearance of reconstructed breasts.
SSM removes breast tissue along with the nipple and areola but leaves most of the breast skin in place. This approach to mastectomy, which retains most of the breast skin and minimizes scarring on the breast, is now widely accepted as oncologically sound in most cases, and when combined with immediate breast reconstruction, makes possible realistic and pleasing results.
Although there are exceptions, most women undergoing treatment for breast cancer and those undergoing prophylactic mastectomy (including BRCA gene mutation carriers) are candidates for SSM surgery. Women seeking even more realistic appearing breasts after mastectomy and reconstruction may want to consider nipple-sparing mastectomy.
» View photographs of the results of breast reconstruction after skin-sparing mastectomy
TDAP Flap

TDAP Flap Breast Reconstruction
Thoracodorsal Artery Perforator flap
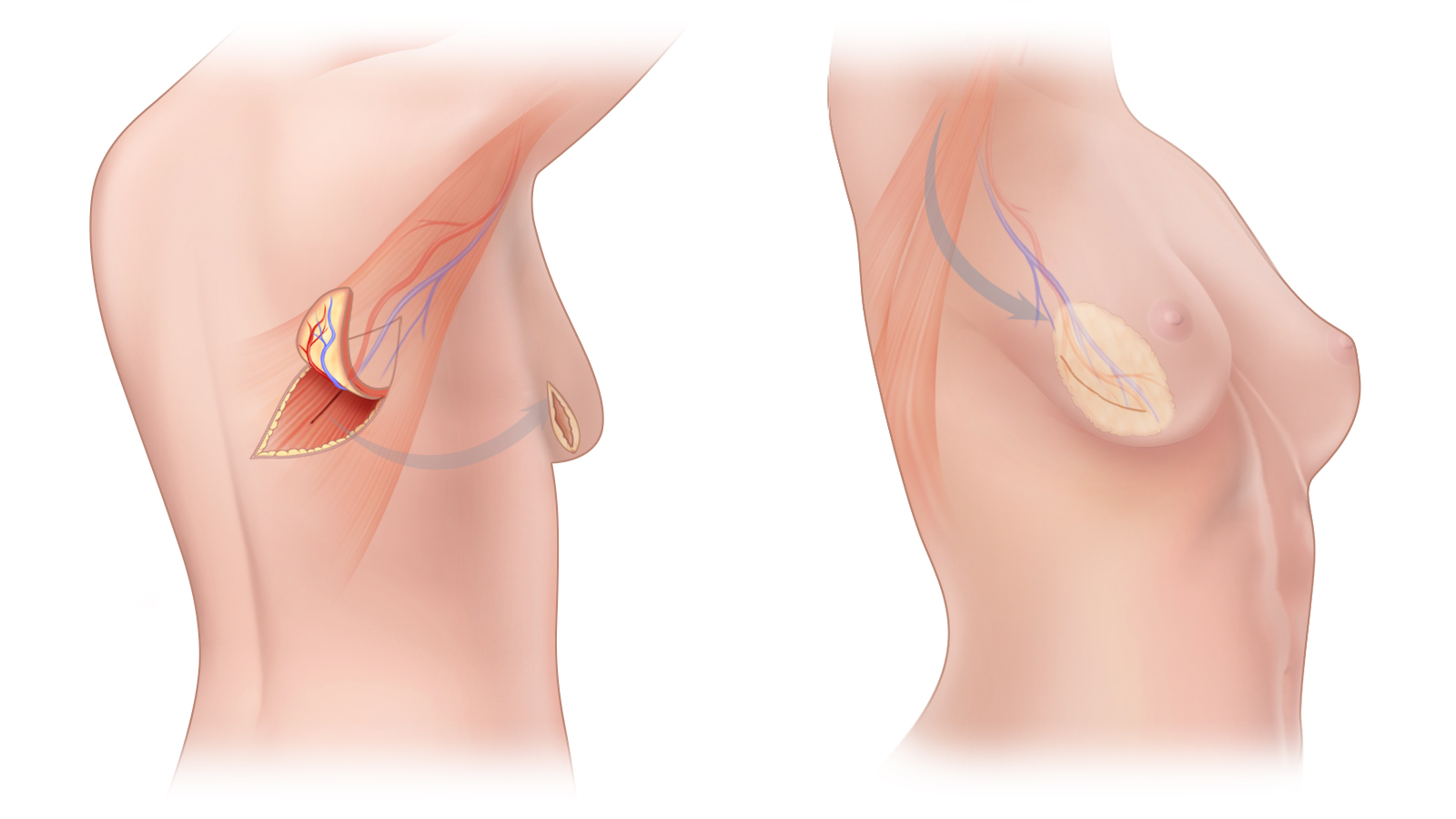
(A) The TDAP flap is a perforator flap composed of skin and fat harvested from the upper back. The blood vessels that supply this flap are meticulously separated from the latissimus dorsi muscle so that muscle is not sacrificed and strength in the arm and shoulder are preserved. (B) The TDAP flap is rotated and “tunneled” under the skin from the back to the chest; microsurgery is not necessary. This flap is commonly used for partial breast reconstruction following lumpectomy and for adding natural tissue to improve the result of a prior breast reconstruction.
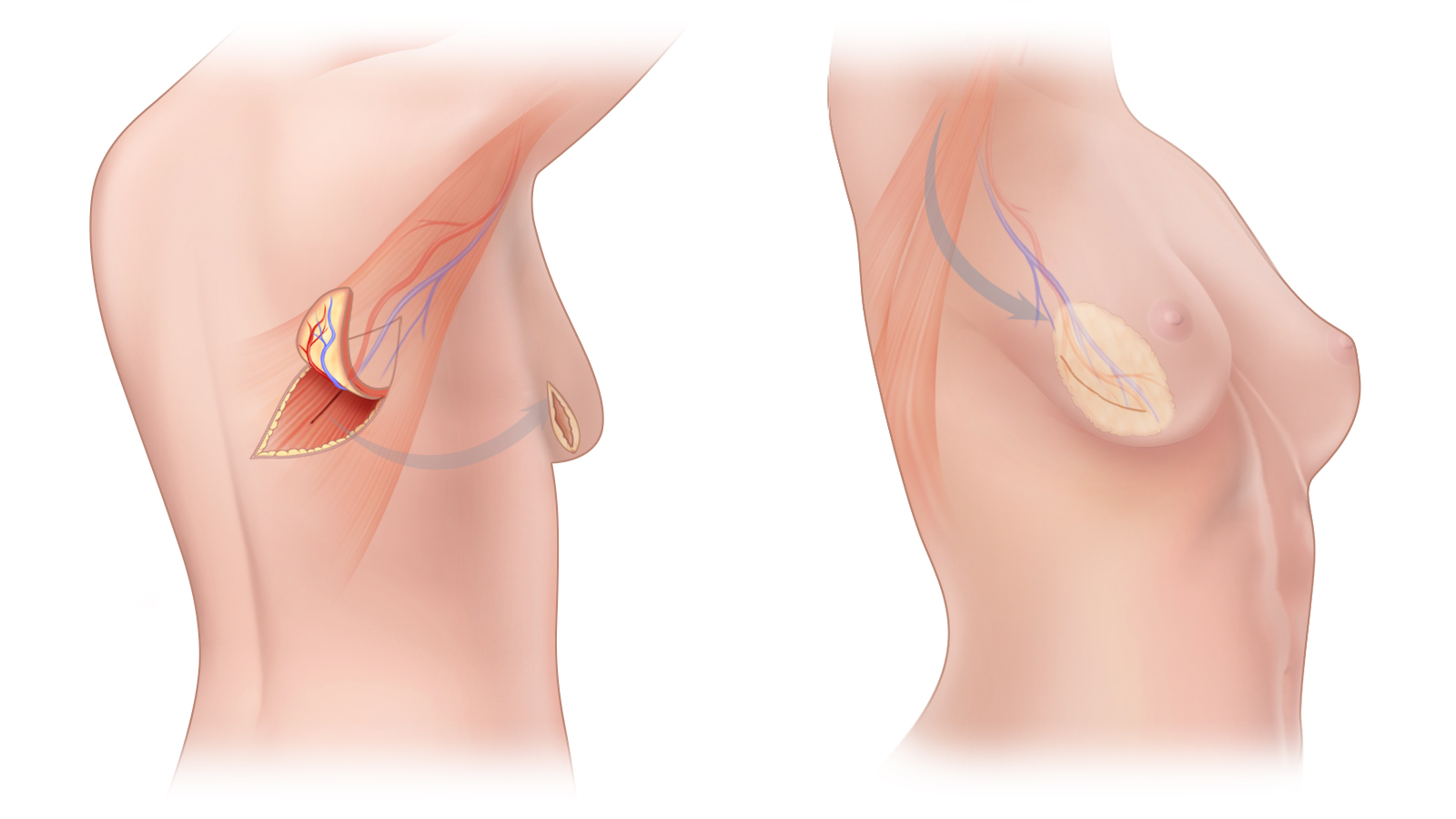
(A) The TDAP flap is a perforator flap composed of skin and fat harvested from the upper back. The blood vessels that supply this flap are meticulously separated from the latissimus dorsi muscle so that muscle is not sacrificed and strength in the arm and shoulder are preserved. (B) The TDAP flap is rotated and “tunneled” under the skin from the back to the chest; microsurgery is not necessary. This flap is commonly used for partial breast reconstruction following lumpectomy and for adding natural tissue to improve the result of a prior breast reconstruction.
The Thoracodorsal Artery Perforator flap, known as a TDAP or TAP flap, is a perforator flap that can be rotated from the upper back in to a position on the chest wall for use in breast reconstruction. TDAP flaps are composed of skin and fat along with the blood vessels that keep the flap alive. These flaps are obtained from the same region of the back as the latissimus dorsi flap, however, no muscle is sacrificed with a TDAP flap. Because these flaps are rotated into place without having to divide and reattach blood vessels, it is not necessary to use the operating room microscope, and most patients only require one night of hospitalization. The preparation of a TDAP flap requires meticulous dissection under loupe magnification. Unfortunately, these flaps are not widely offered as an option to women undergoing breast reconstruction.
Although most women do not have enough tissue on the upper back to enable the surgeon to use TDAP flaps alone for breast reconstruction after mastectomy, these flaps are an excellent way to supplement an existing breast reconstruction with additional volume without the need for breast implants or other kinds of flaps. TDAP flaps can also be used as an alternative to implants in the correction of tubular beast deformity and as an option for women who want to undergo breast augmentation using their own tissue. The scar that results from TDAP flaps can generally be placed horizontally along the bra line so that it can be covered up by a bra.
TDAP Flap Breast Reconstruction in New York and Connecticut
Contact us to schedule a consultation or if you would like more information about the options for breast reconstruction after mastectomy including TUG flaps, DIEP flaps, SIEA flaps and SGAP flaps. Our practice has offices in Manhattan and Greenwich, Connecticut.
Your Rights

Breast Reconstruction: Your Rights
A number of laws in the United States protect a woman’s right to obtain insurance coverage for breast reconstruction surgery. In addition, Federal law now also protects you against discrimination by health insurance companies and employers on the basis of genetic information such as BRCA status.
Federal Law and Breast Reconstruction
If you have had a mastectomy, or expect to have one, you should be aware of the Women’s Health and Cancer Rights Act of 1998 (WHCRA). This federal law insists that group health plans and individual health policies that provide coverage for mastectomies also provide coverage for breast reconstruction in connection with such mastectomy.
Under WHCRA, group health plans, insurance companies and health maintenance organizations (HMOs) offering mastectomy coverage also must provide coverage for certain services relating to the mastectomy in a manner determined in consultation with your attending physician and you. This required coverage includes all stages of reconstruction of the breast on which the mastectomy was performed, as well as surgery and reconstruction of the other breast to produce a symmetrical appearance.
Read the Women’s Health and Cancer Rights Act of 1998 (WHCRA).
Federal Antidiscrimination Law and Your Genetic Information
Some women have been afraid to proceed with elective treatment such as BRCA genetic testing or prophylactic mastectomy because they fear that the data about them—for example, that they are carriers of a genetic mutation that predisposes them to developing breast cancer—might be used against them on the job or in some other way. In fact, these recent U.S.laws provide protection against such mis-use of medical information.”]
On May 21st, 2008 the Genetic Information Nondiscrimination Act (GINA) was signed into Federal law. This law prohibits discrimination in health coverage and employment based on genetic information about an individual and the genetic information of family members. The GINA spells out unlawful practices in the use of genetic information for health insurers, employers, employment agencies, labor organizations, and employment training programs.
More specifically, GINA strictly prohibits the following:
Health Insurance Issues
- Health insurers may not require individuals to provide their genetic information or the genetic information of a family member to the insurer for eligibility, coverage, underwriting, or premium-setting decisions. However, a health insurer may request that an individual provide genetic information if coverage of a particular claim may be appropriate only if there is a known genetic risk—for example, if you want your insurance company to cover a prophylactic mastectomy because you have found that you are a carrier of the BRCA gene.
- Health insurers may not make enrollment or coverage decisions using genetic information collected either intentionally or incidentally.
- Health insurers may not request or require that an individual or an individual’s family member undergo a genetic test.
- In the Medicare supplemental policy and individual health insurance markets, genetic information cannot be used as a preexisting condition.
Employment Issues
- Genetic information may not be used in making decisions regarding hiring, promotion, terms or conditions, privileges of employment, compensation, or termination.
- An employer, employment agency, labor organization, or training program may not limit, segregate, or classify an employee or member, or deprive that employee or member of employment opportunities, on the basis of genetic information.
- An employer, labor organization, or joint labor-management committee may not use genetic information in making decisions regarding admission to or employment in any program for apprenticeship or training and retraining, including on-the-job training.
State Laws and Breast Reconstruction
In addition to the protections afforded by the Federal 1998 WHCRA, most states have laws pertaining to insurance coverage for breast reconstruction surgery.
Read more about your state’s laws.
Insurance Coverage for Breast Reconstruction

Insurance Coverage for Breast Reconstruction
The surgeons of the Advanced Reconstructive Surgery Group are participating providers in many major insurance plans including:
- United Health Care
- Oxford Health Plans
- Anthem Blue Cross Blue Shield (CT) (Dr. Erhard)
- Cigna
- Connecticare
- MVP
- The Empire Plan (NYSHIP)
- Medicare (Dr. Erhard and Dr. Lamelas)
We are continually trying to work with other insurers to increase the number of networks in which we participate. If you are insured by a plan with which we do not participate, please know that our staff is very experienced in working with insurers to help you obtain coverage for breast reconstruction procedures.
In almost all cases, if your insurance plan provides coverage for the cost of a mastectomy it must also, according to Federal law, provide coverage for the method of breast reconstruction you wish to undergo. Coverage for reconstruction includes all methods of reconstruction, including breast implants and natural-tissue breast reconstruction options such as the DIEP, LAP, and PAP flaps. If a surgeon in your network of participating providers does not offer the method of reconstruction you prefer, your insurer must generally still provide coverage, even if this means the insurer must cover the cost of surgery with a “non-participating” physician.
We are frequently able to obtain authorizations for women who do not have access to “in-network” physicians offering the most sophisticated methods of natural-tissue perforator flap breast reconstruction to go out of their networks for surgery. We are often able to arrange for coverage, on an individual basis, for women with HMO plans, patients with self-funded ERISA plans, people who have previously been denied coverage for breast reconstruction surgery and for women with unsatisfactory outcomes from prior reconstruction. In all cases, we will work closely with you and your insurance carrier to minimize any out-of-pocket expenses.
For more information, please contact our office at 203-863-0003.
Overview of Federal Law Pertaining to Breast Reconstruction
A more comprehensive description of State and Federal laws pertaining to breast reconstruction surgery can be found in the Your Rights section of this site.
The Women’s Health and Cancer Rights Act (WHCRA) of 1998 contains important protections for women who wish to have breast reconstruction after mastectomy. This law requires group health plans and individual health policies that provide coverage for mastectomies to also provide coverage for breast reconstruction.
In accordance with the WHCRA, members of group health plans receiving mastectomy-related services are entitled to:
- Reconstruction of the breast on which the mastectomy has been performed
- Surgery on the opposite breast to produce a symmetrical appearance (including reduction, breast lift or augmentation)
- Treatment of physical complications at all stages of the mastectomy, including lymphedema
Additional information is available from the US Department of Labor, which has oversight of the WHCRA.
» Contact us if you would like more information or to schedule a consultation
DIEP Flap Myths

Myths About DIEP Flaps, Perforator Flaps and Breast Reconstruction
- MYTH: The DIEP flap is an experimental procedure.
-
DIEP flap surgery is not considered experimental. Since fewer surgeons have been trained to perform perforator flap breast reconstruction than other methods of reconstruction, TRAM flap and implant reconstructions are more widely available. The DIEP flap was developed in the late 1980s and has been used extensively for breast reconstruction since the early 1990s. In fact, Dr. Greenspun is an author of a published scientific paper reviewing almost 4000 perforator flap breast reconstructions.
- MYTH: DIEP flap (or other perforator flap) surgery takes a long time to perform, and is therefore risky, dangerous and difficult to recover from.
-
When performed by experienced surgeons, DIEP flaps and other perforator flap breast reconstructions are not riskier than other methods of breast reconstruction. Although perforator flap surgery can take longer in the operating room than implant reconstructions, published studies in peer-reviewed journals have found that, in the hands of an experienced microsurgeon, the time it takes to perform a perforator flap reconstruction is generally rewarded with excellent short- and long-term results. In fact, better surgical outcomes have been noted in a number of regards. For example, the chances of developing a hernia following a TRAM flap is reported in the medical literature to range from about 3% to about 30%, but about 1% following a DIEP flap.
Unlike surgery on the intestines, gallbladder, or other internal organs (such procedures are known as “intra-abdominal”), perforator flap breast reconstruction takes place in the more superficial layers of the body. While long intra-abdominal surgeries are often associated with difficult and prolonged recovery, perforator flap surgery generally means a relatively rapid recovery. Although perforator flap surgery takes significantly longer to perform than tissue expander/implant reconstruction, in many ways the body’s response to undergoing a DIEP flap breast reconstruction more closely resembles the response to a breast reduction or a tummy-tuck than to major intra-abdominal surgery. It is not uncommon for patients who undergo perforator flaps to be out of bed and sitting in a chair on the first day after surgery, and to be walking around by the second day following surgery.
- MYTH: DIEP flaps have a higher complication rate than other types of breast reconstruction.
Every surgical procedure carries some degree of uncertainty and risk. However, studies published in peer-reviewed journals such as the Journal of Plastic and Reconstructive Surgery, Journal of Reconstructive Microsurgery, Annals of Plastic Surgery and British Journal of Plastic Surgery have repeatedly demonstrated the safety of DIEP flap breast reconstruction.
Data published by the implant manufacturer Mentor in their patient labeling “Saline-Filled Breast Implant Surgery: Making an Informed Decision” outlines the findings of their study of saline filled implants required by the United States Food and Drug Administration (FDA). The data below have been extracted from the publication, which is available in its entirety on the website of the FDA along with the publications for other approved breast implants.
You can compare the safety of DIEP flap surgery to implant reconstruction by looking at the published data below:IMPLANT RECONSTRUCTION COMPLICATIONS AT 5 YEARS AT 7 YEARS AT 10 YEARS Unanticipated Reoperation 43% 50% 56% Removal of Implant 30% 39% 45% Capsular Contracture (Grade III, IV or unknown) 29% 49% 59% Implant Deflation 18% 27% 33% Breast Pain 16% 29% 37%
Your Rights section of this site.(Adapted from Mentor publication “Saline-Filled Breast Implant Surgery: Making an Informed Decision” – available through the FDA)DIEP FLAP COMPLICATIONS AT 10 YEARS Unanticipated Reoperation 5.96% Hernia 0.75% Total Flap Failure Approximately 1% (Adapted from “A 10-Year retrospective review of 758 DIEP Flaps for Breast Reconstruction” published in Plastic and Reconstructive Surgery)
Comparison to published rates for DIEP flap complications shows that women who undergo reconstruction with an implant are up to 7 times more likely to have an unanticipated surgery to address a complication of their reconstruction. The risk of complications associated with the use of an implant is even higher when radiation is part of a woman’s treatment.
- MYTH: Recovery after DIEP flap surgery is more painful and difficult than after other types of breast reconstruction.
Cutting across the fibers of a muscle (which will cause the muscle to go into spasm), or over-stretching a muscle with a tissue expander can cause significant pain and discomfort. Since it is not necessary to cut across muscle fibers or put muscle under stretch with perforator flap breast reconstruction surgery, it is not surprising that women who undergo these procedures are quite comfortable after surgery. It is not uncommon for patients to report that they had “much less pain” after their DIEP flap than after their C-section. Studies have show that women who undergo DIEP flaps have less postoperative pain and discomfort and more rapid recovery than women who undergo TRAM flap surgery.
- MYTH: It is often necessary, during surgery, to convert from a DIEP flap to a TRAM flap because of “issues with blood vessels” or “because it is safer.”
Although some surgeons who perform DIEP flap surgery frequently convert to a free TRAM flap procedure during surgery, Dr. Greenspun relies upon preoperative imaging of blood vessels to plan surgery in advance, and thus avoid the need the need to “change-over” to a muscle-sacrificing procedure during surgery. Dr. Greenspun pioneered the use of MRI for imaging of perforator flap blood vessels, and he has published extensively on the topic. In Dr. Greenspun’s opinion, rarely, if ever, should conversion to a free TRAM flap be necessary.
- MYTH: Because I have had other abdominal surgery, I am not a candidate for a DIEP flap.
Most women who have had prior abdominal surgery (including C-sections, hysterectomies, gall bladder removal, laparotomy, appendectomy, tubal ligations, laparoscopic and even some liposuction procedures) are still candidates for DEIP flap surgery. Occasionally, prior surgery may have damaged the blood vessels needed for a DIEP flap, and some surgeons therefore routinely suggest that abdominal perforator flap surgery is contraindicated in patients with a history of previous abdominal surgery. The development of reliable preoperative blood vessel imaging means that it is now possible to locate suitable vessels and perform DIEP flap breast reconstructions in almost all women who have had prior surgery. In situations when all suitable abdominal vessels have been damaged by prior surgery, an alternate perforator flap such as a GAP or LAP flap can generally be selected for breast reconstruction.
- MYTH: Because I am thin, I am not a candidate for DIEP flap or other perforator flap breast reconstructions.
Many thin women are candidates for a DIEP flap breast reconstruction. Even very thin women are often candidates for this type of breast reconstruction because breast and abdominal size tend to be proportionate. We have found that even women who have previously been told that they are too thin to have a DIEP flap, have successfully been reconstructed with DIEP flaps. Preoperative imaging of blood vessel helps to make this possible. When a woman’s abdomen cannot provide enough tissue to reconstruct breasts of her desired size, it is usually possible to reconstruct the breasts using a flap taken from the buttocks (GAP), “love handle” area (LAP) or inner thigh (TUG).
- MYTH: Because I am overweight, I am not a candidate for DIEP flap or other perforator flap breast reconstruction.
Being overweight is not itself a contraindication to perforator flap breast reconstruction. Following a comprehensive medical workup and evaluation, we routinely operate on patients who are overweight. Some complications occur at a higher rate in obese patients, however, with appropriate planning, perforator flap surgery can still be an option for breast reconstruction.
- MYTH: There is not much difference between a TRAM flap and a DIEP flap.
Although both the TRAM flap and the DIEP flap use soft tissue from the lower abdomen to reconstruct a breast, there are major differences in the way these two procedures affect the abdomen after surgery. Since TRAM flaps remove muscle from the abdominal wall, and DIEP flaps do not, the former are associated with significantly more postoperative pain and a longer period of recovery. Women reconstructed with TRAM flaps have been found, in the long term, to suffer from diminished trunk strength and a much higher incidence of hernias and bulges than women who undergo DIEP flap breast reconstruction. Because muscle is not sacrificed with a perforator flap, strength is well preserved.
- MYTH: I am not a candidate for DIEP flap or other perforator flap breast reconstruction because I am “too old”.
There is no particular age at which a woman is too old to undergo perforator flap breast reconstruction. A woman’s age will be one of many factors that determine whether she is a good candidate for a DIEP or other perforator flap breast reconstruction. In general, a woman’s overall heath is a much more important measure of her suitability for surgery than her age.
- MYTH: Although I have problems with my implant reconstruction, I cannot have a DIEP flap because my insurance company will only cover the expense of the initial surgery.
The 1998 Federal Breast Reconstruction Law (also known as the Women’s Health and Cancer Rights Act) requires insurance providers to provide coverage for breast reconstruction surgery following mastectomy as well as any surgery necessary to create symmetry in either breast. Additional surgery, including replacing an implant used in breast reconstruction with a DIEP or other perforator flap, needed to address problems with an implant reconstruction is considered medically necessary. Our office can help you to secure authorization for such surgery.
- MYTH: I cannot have a DIEP flap or other perforator flap because there is not a plastic surgeon in my area that performs these procedures.
Most plastic surgeons do not perform perforator flap breast reconstruction because of its complexity. These microsurgical procedures are technically difficult and time consuming. The best success rates and the highest degree of efficiency are achieved when these reconstructive procedures performed by a team of experienced microsurgeons. There are very few microsurgical breast reconstruction teams committed to such an endeavor. If you do not have access to doctors who perform perforator flap reconstruction in your community, your insurance carrier typically is obligated to find you a surgeon who can provide you with the reconstruction method of your choice. This means you may be granted a “gap-in-coverage” or “out-of-network” exception to see a specialist who can provide the service for you.
Our office is accustomed to taking care of out-of-town patients who come to us to undergo DIEP flap or other perforator flap breast reconstructions in New York City or Greenwich Connecticut. We can help coordinate your travel plans and stay in either location. If you have recently been diagnosed with breast cancer, our staff can help arrange prompt consultation with one the breast oncologic surgeons with whom Dr. Greenspun works. If necessary, we can also arrange consultations for you with medical and radiation oncologists who, together with Dr. Greenspun and your breast surgeon, will develop a comprehensive cancer treatment plan.
- MYTH: My insurance company will not pay for a DIEP flap or pther perforator flap.
As a result of the Women’s Health and Cancer Rights Act of 1998, health insurance carriers are required to cover the expense of breast reconstruction following mastectomy. This Federal Act also protects a woman’s right to select the type of reconstruction she wishes to undergo. Most insurance plans are happy to have patients pursue expander/implant reconstructions and the older methods of flap reconstruction such as the TRAM flap, as they generally have network-participating surgeons who perform these procedures. An insurer cannot, however, deny coverage for a breast reconstruction procedure such as a DIEP flap simply because they do not have a network-participating physician willing or able to perform the breast reconstruction procedure a woman wishes to have.
Our office has extensive experience obtaining out-of-network exceptions for women who wish to undergo perforator flap breast reconstruction but do not have access to a network-participating physician who performs these procedures. We are often able to obtain these exceptions both for patients with HMO plans and for those who have out-of-network benefits but prefer to try to stay within their networks. In all cases, we will work closely with you to minimize your out-of-pocket expenses for surgery.
- MYTH: Most plastic surgeons perform DIEP flap breast reconstructions.
-
Although the websites of many plastic surgeons describe DIEP flap breast reconstruction, most plastic surgeons do not routinely perform these or other types of perforator flap breast reconstruction even if they perform microsurgery. In part, this is because most plastic surgery training programs do not provide significant exposure to these complex reconstructive procedures, but do provide extensive training in implant and TRAM flap reconstructions.
If you are considering perforator flap breast reconstruction, you may want to find out more information about your doctor’s experience with these procedures. Here are some useful questions to consider asking:- Are you certified by The American Board of Plastic Surgery® or The Royal College of Physicians and Surgeons of Canada®?
- Have you had additional training in microsurgery and perforator flap breast reconstruction after residency?
- What types of breast reconstruction do you most commonly perform?
- How many DIEP flap procedures have you performed?
- How many DIEP flap procedures did you perform last week/month/year?
- How often do you convert a DIEP flap to a free TRAM flap?
- What is your success rate?
- Who, if anyone, will your assistant surgeon be?
- Who will be monitoring my flap after surgery?
It is also a good idea to review a significant number of postoperative photographs of the surgeon’s patients who underwent perforator flap breast reconstruction. This will help you to get a sense of what reconstructed breasts look like and to know more about your doctor’s results in particular.
Breast Reconstruction in New York and Connecticut
Our practice specializes in the most advanced methods of natural-tissue breast restoration. Certified by the American Board of Plastic Surgery, Dr. Greenspun specializes in microsurgical breast reconstruction surgery including DIEP flap, SIEA flap, SGAP flap, IGAP flap, LAP flap and TUG flap surgery. Our offices are located in New York City and Greenwich, Connecticut.
Our Practice

Breast Reconstruction Experts
Exceptional and Personalized Patient-Focused Care
The surgeons of the Advanced Reconstructive Surgery Group are breast reconstruction subspecialists.
Our highly specialized practice is specifically devoted to the most innovative and advanced methods of restorative breast surgery. Our mission is to help women fighting breast cancer, or undergoing risk-reducing preventative mastectomy, restore their bodies, and their lives.
Amongst the plastic and reconstructive surgeons of our team are respected leaders and pioneers in the most advanced methods of breast reconstruction and microsurgery. Together, Drs. David Greenspun and Heather Erhard have performed over 1,000 microsurgical perforator flap breast reconstruction procedures with a roughly 99.5% or better success rate. Their reputation puts them amongst the most trusted breast reconstruction specialists anywhere in the world, and therefore our practice regularly welcomes out-of-state and international patients. Dr. Andreas Lamelas recently joined our team from Harvard University; his focus is on breast reconstruction and on treating lymphedema associated with breast cancer treatment.
The Surgeons of the Advanced Reconstructive Surgery Group believe in shared decision making and believe that different approaches to breast reconstruction are right for different people. In addition to natural-tissue breast reconstruction, reconstruction using breast implants is a regular part of the group’s practice.
The doctors of the Advanced Reconstructive Surgery Group are in-network with many major health insurance plans including:
- United Health Care
- Oxford Health Plans
- Cigna
- Blue Cross-Blue Shield (Anthem and others)
- Connecticare
If you plan to have your breast cancer treatment in New York City or Connecticut, our staff can help coordinate all aspects of your care with a multidisciplinary team of specialists, including medical oncologists and radiation oncologists who work with our tor breast reconstruction surgerons. Contact us if you would like to make an appointment and learn more about your options
Terms of Use

This site, and its content, is intended to provide general information for informational and educational purposes only. This site is not an attempt to practice medicine or provide specific medical advice or opinion. This site should not be used to make a diagnosis nor should it be used to determine a course or specific method of treatment. This site should not and cannot replace a qualified healthcare practitioner’s care and judgment. This site is provided as-is with no representations or warranties, either express or implied or otherwise including, but not limited to, warranties of title, fitness for a particular purpose, merchantability or non-infringement. We do not make any representations, assurances, warranties or guarantees related to our website or to websites linked to or from this site. We strongly encourage all users to consult with a qualified healthcare professional for any health or medical questions or concerns.
Links to other sites are provided only as a courtesy to visitors to this site. These links do not constitute an endorsement of products, services or information provided by other sites. The inclusion of links to other sites does not imply that the other sites have given permission for inclusion of these links, or that there is any relationship between David T. Greenspun, M.D. and the linked site. David T. Greenspun, M.D. is not responsible for the privacy practices or the content of others web sites.
While we try to keep the information of this site as accurate as possible, we disclaim any warranty concerning its accuracy, completeness, correctness and timeliness, and disclaim any other warranty, express or implied, statutory or otherwise. The content of this site is provided solely as a convenience to visitors of this site without warranty of any kind, either express or implied. You understand and agree that use of this site is at your sole risk and that the content of this website is provided by David T. Greenspun, M.D., P.C. on an “as-is” basis. You assume full responsibility for using this site and the information provided on and through this site and you understand and agree that David T. Greenspun, M.D., his associates, employees and affiliates are not responsible or liable for any claim, loss or damage from its use by you or any user. David T. Greenspun, M.D., his agents, associates, employees and affiliates shall in no way be liable to you or any third person or entity for any loss or injury or for any direct, indirect, incidental, special, punitive, consequential or any other damages whatsoever arising out of or otherwise resulting from the use of this website, or the use of the websites accessed from links on this website including, without limitation, with regard to any errors, omissions or inaccuracies of information and content, any unauthorized access to or use of this site’s secure servers and/or any and all personal information stored therein, or that may result from any person following the information offered or provided on this website. The foregoing limitation of liability includes, but is not in any way limited to, any and all economic loss, personal injury, illness or death or loss, liability or damage of any kind, whether based on warranty, contract, tort, or any other legal theory, and whether or not David T. Greenspun, M.D. is advised of the possibility of such damages. The foregoing limitation of liability shall apply to the fullest extent permitted by law. By accessing or using our website you agree to indemnify, defend and hold harmless David T. Greenspun, M.D., his associates, employees and affiliates and each of their managers, members, officers, directors, shareholders, employees and agents, from and against all liabilities, losses, expenses, damages and costs (including attorneys’ fees), resulting from the use of this site, either directly or indirectly.
Use of this site or communication through this site with David T. Greenspun, M.D., does not establish or constitute a doctor-patient relationship. Although reasonable efforts will be made to protect the confidentiality and security of information submitted to us through this site, information submitted does not constitute protected health information (PHI) as defined by the regulations of the Health Insurance Portability and Accountability Act (HIPAA), as this website does not provide medical advice or care, nor does communication through this site establish a doctor-patient relationship.
Your privacy and the confidentiality of your personal information is important to us, however, by its very nature, a website cannot be absolutely protected against intentional or malicious intrusion attempts. Similarly, David T. Greenspun, M.D. does not control the devices or computers or the internet over which you may choose to send confidential personal information and therefore, cannot prevent such interceptions of compromises to your information. Consequently, while we will attempt to keep your information secure, David T. Greenspun, M.D. hereby makes no guarantee as to security, integrity or confidentiality of any information transmitted to or from this website, or stored within this website. In addition, we hereby make no guarantee as to security, integrity or confidentiality of any information transmitted to or from this website or any associated email addresses.
When you send an electronic mail transmission or other electronic communication including, but not limited to, electronic mail and completed electronic forms, the electronic transmission is not necessarily secure. Accordingly, electronic transmission of information, including electronic mail transmission, is not necessarily protected from unauthorized access. Consequently, any electronic communication made with David T. Greenspun, M.D., his agents, associates, employees and affiliates through this web site is made at your own risk. Transmission of email and other forms of electronic communication are at your own risk and will be considered to constitute your authorization to receive electronic, written or oral communication from David T. Greenspun, M.D., his agents, associates, employees and affiliates in response to your communication. David T. Greenspun, M.D., his associates, employees and affiliates and each of their managers, members, officers, directors, shareholders, employees and agents cannot and do not accept responsibility for your transmission of confidential information and disclaim any obligation with respect to that information. You assume the sole risk of transmitting your information as it relates to the use of this website, and for any data corruptions, intentional interceptions, unintentional interceptions, intrusions or unauthorized access to information, or of any delays, interruptions to or failures preventing the use this website.
This site should never be used for urgent or emergent communication with our offices or with David T. Greenspun, M.D.
The content of this web site is intended for general informational and educational purposes only and is not a substitute for professional advice provided by a physician, attorney, accountant or licensed financial or legal professionals. Information on this site does not constitute medical, financial or legal advice or opinion. In no event shall David T Greenspun, M.D., his associates, employees and affiliates and each of their managers, members, officers, directors, shareholders, employees and agents be liable for any direct, indirect, special, consequential or monetary damages, including fees, and penalties in connection with your use of materials posted on this site or connectivity to or from this site to any other site.
The content of this website is protected by copyright law. Permission to reprint or otherwise reproduce any information contained on this site, in whole or on part, is prohibited, unless prior written consent is obtained. We do not warrant that access to this site will be error- free or virus-free. Photographs of actual patients of David T. Greenspun, M.D.,used with permission, appear in this website and are marked as such; other photographs used in this website are of models and are not patients of David T. Greenspun, M.D. The display of photographs of patients is intended for general informational and educational purposes only. Individual results vary based upon a number of factors including body type, age, breast size and lifestyle and consequently, the results shown are not a guarantee.
Your use of this website constitutes your acknowledgement of and agreement to the terms of use. We reserve the right to periodically modify terms, conditions and policies, without notice to you, and therefore suggest that you periodically review them. This notice outlines our Terms of Use and privacy practice for visitors to our web site and is distinct from our Notice of Privacy Practices for Protected Health Information. Our practice specializes in perforator flap breast reconstruction including DIEP flaps in New York City, Manhattan, New York as well as Greenwich and Stamford, Fairfield County, Connecticut.
Hospitals and Facilities

Breast Reconstruction in Connecticut & New York
Hospitals and Facilities
The breast reconstruction specialist surgeons of the Advanced Reconstructive Surgery Group offer microsurgical perforator flap breast reconstruction, including DIEP flaps, Stacked DIEP flaps, Lumbar Artery Perforator flaps, Body Lift Breast Reconstruction and breast reconstruction using breast implants in Connecticut and New York.
Breast reconstruction surgery is (DIEP, LAP, PAP, other perforator flaps, and breast implant reconstruction) performed in one the Metropolitan Area hospitals with which our doctors are affiliated.
Our Hospitals include:
Greenwich Hospital—an American College of Surgeons Accredited Cancer Center and Yale-New Haven System affiliate,
Stamford Hospital in Stamford Connecticut—a Columbia University affiliate hospital
Vassar Brothers Medical Center in Poughkeepsie, NY
Danbury Hospital in Danbury, CT
Northern Dutchess Hospital in Rhinebeck, NY
The New York Eye and Ear Infirmary—a Mt. Sinai affiliate
Weiler Hospital of the Albert Einstein College of Medicine
At all of our affiliated hospitals, a skilled team of expertly trained medical professionals (including surgeons, anesthesiologists, oncologists and nurses) will help assure that you receive the best possible care.
Travel Information

Travel Information
If you will be coming from out of town for breast reconstruction surgery, our office staff can assist you in making travel arrangements to New York City or Fairfield County, Connecticut. We recognize that traveling to undergo treatment may be stressful. Our goal is to make sure that any inconvenience is minimized so that you can stay focused on healing. If you would like our office to assist you with travel plans, please let us know.
Getting to Us
By Air
Most of our patients travel to and from their care with us on commercial airlines, and John F. Kennedy (JFK), LaGuardia (LGA), Westchester (HPN) and Newark (EWR) airports are all relatively close by.
Patients who will travel by air to undergo treatment may be able to travel at no cost using the Corporate Angel Network or Angel Flight. The Corporate Angel Network is a charitable organization that arranges free travel on corporate jets for patients traveling to or from an approved cancer centers. Angel Flight is a non-profit charitable organization of pilots and volunteers that arranges free air transportation for medically related treatment. Our office can help you make arrangements with these no-cost flights. Air Charity Network provides free airline travel for patients with both medical and financial needs. Visit their website at aircharitynetwork.org or call (877) 621-7177 for more information.
By Rail
The Northeast corridor rail lines include stops in our area. Amtrak services Penn Station and Stamford Connecticut while MetroNorth services Greenwich, Stamford and Poughkeepsie.
Accommodations
For out-of-town patients who wish to have their surgery at Greenwich Hospital, arrangements can be made for you and anyone accompanying you to stay at an area hotel or local bed and breakfast. A number of hotels in the area offer special rates for patients undergoing treatment at Greenwich Hospital. Greenwich, is a lovely Fairfield County, Connecticut town just next to Stamford, Connecticut. Less than 40minutes by train from New York City’s Grand Central Station, Greenwich provides visitors with access to parks, museums, seashore, dining, shopping and the arts. You can visit the official website of the Town of Greenwich, Connecticut or the website of the Greenwich Chamber of Commerce for more information.
Stanton House Inn, Greenwich, CT
Hyatt Regency, Greenwich, CT
Hampton Inn & Suites, Stamford, CT
Holiday Inn Express Stamford, CT
Contact us if you would like assistance in making travel plans for your treatment
Our Breast Surgery Team

New York & Connecticut Breast Reconstruction Teams
DIEP Flap Surgeons
Dr. Greenspun’s experienced, skilled and dedicated team takes care of our patients before, during and after surgery. The team includes office personnel, other highly skilled physicians, nurses and surgical technicians.
For women who will undergo an immediate reconstruction (mastectomy and reconstruction performed during the same procedure), the team will also include a board certified breast surgeon. In addition to the breast surgeons in New York City with whom we work, our team of breast surgeons include Barbara Ward, MD, Alyssa Gillego, MD—both are affiliated with the Breast Center at Greenwich Hospital—as well as Susan Boolbol, MD and Carinne Anderson, MD—who are affiliated with the Dyson Center for Cancer Care at Vassar Brothers Medical Center. These breast specialists offer the most advanced treatments for breast cancer, including skin-sparing mastectomy and nipple-preserving or nipple-sparing mastectomy in conjunction with immediate perforator flap breast reconstruction.
If you plan to have your full breast cancer treatment in New York City or Connecticut, our staff can help coordinate all aspects of your care with a multidisciplinary team of specialists, including medical oncologists and radiation oncologists. Contact us if you would like to make an appointment and learn more about your options
About Dr. Greenspun

About Dr. Greenspun
Breast Reconstruction Specialist - New York and Connecticut
Breast Reconstruction Specialist - New York and ConnecticutDavid T. Greenspun, MD, MSc, FACS is a Board Certified Plastic Surgeon specializing in breast reconstruction. Dr. Greenspun has earned the reputation of being an internationally recognized expert in the field of microsurgical breast reconstruction. He has pioneered new techniques in the field and has successfully performed approximately 1,000 perforator flap breast reconstructions.
Dr. Greenspun is an Associate Editor for the Breast Reconstruction Section of the American Society of Plastic Surgeons’ Plastic Surgery Education Network. Dr. Greenspun has numerous textbook chapters, articles and peer-reviewed studies about breast reconstruction to his credit, and is frequently an invited speaker at medial meetings and conferences
With a decade and a half of experience as a specialist in the most advanced methods of breast reconstruction, he makes exceptional and personalized care the backbone of his practice. Aesthetic excellence in breast reconstruction is a primary objective. By combining the most sophisticated techniques of reconstructive surgery with the principles of aesthetic surgery and artistry, he has achieved distinction amongst patients and colleagues alike.
Dr. Greenspun and his team are renown for revolutionary reconstructive techniques such as the lumbar artery perforator flap for breast reconstruction, and for “body-lift breast reconstruction” using extended DIEP flaps—a technique that allows some thin women to have a breast reconstruction using abdominal tissue when a traditional DIEP flap would not be adequate. In addition, Dr. Greenspun has developed and refined techniques that allow some women who would not otherwise be candidates for nipple-sparing mastectomy to successfully have this type of surgery.
Dr. Greenspun received a Bachelor of Science degree with distinction from McGill University in Montreal. While at McGill, he received a grant from Fonds de recherche en santé du Québec (Province of Quebec Funds for Research in Health) to conduct advanced research at the Montreal Neurological Institute; he was awarded a Master of Science degree for this work. Subsequently, Dr. Greenspun returned to his home state and received his Doctorate of Medicine degree with High Honors from the University of Medicine and Dentistry of New Jersey, and was admitted to the Alpha Omega Alpha National Medical Honor Society.
Dr. Greenspun trained in general surgery at New York Presbyterian Hospital-Cornell Medical Center and trained in plastic and reconstructive surgery at the Albert Einstein College of Medicine-Montefiore Medical Center. Dr. Greenspun is certified by the American Board of Plastic Surgery. He is a Fellow of the American College of Surgeons and a member of both the American Society of Plastic Surgeons and the American Society for Reconstructive Microsurgery. He holds clinical appointments at New York City hospitals including the New York Eye and Ear Infirmary, Saint Luke’s-Roosevelt Hospital, Vassar Brothers Medical Center and Montefiore Medical Center, Saint Barnabas Hospital in New Jersey as well as at Greenwich Hospital and Stamford Hospital in Connecticut.
Dr. Greenspun lives in Greenwich, CT with his children and wife, Rachel Schneider. He enjoys skiing and exercise. He is an avid photographer and loves to cook.
Download Dr. Greenspun’s Curriculum Vitae
» Contact us if you would like to make an appointment and learn more about your options
Surgical Risks

Surgical Risk
Unfortunately, there is no risk-free method of breast reconstruction available. Anyone considering surgery must weigh the pros and cons of the possible procedures, and should consider any possible alternatives. In addition to the general risks associated with any surgical procedure—for example, the possibility of infection—there is some risk that is unique to the microsurgical nature of perforator flap surgery. While the success rate of these procedures in the hands of experienced surgeons who regularly perform these procedures is extremely high—in the range of 99%—the small vessels that nourish free flaps can become compromised, possibly leading to the loss of a flap. In spite of this small but real risk, perforator free flaps are an invaluable option for breast reconstruction because of the significant advantages these flaps have. They produce excellent aesthetic results with very low incidence problems at the donor site and of unplanned reoperation.
Our patients know that having a highly qualified medical team is of supreme importance. Every surgical procedure carries some degree of uncertainty and risk. Dr. Greenspun will use his skills and expertise to avoid complications insofar as is possible. If a complication does occur, he and his team will use those same skills to attempt to solve the problem as proficiently and as quickly as possible to help you achieve your reconstructive goals.
Contact us if you would like to make an appointment and learn more about your options for breast reconstruction after mastectomy.
Breast Reconstruction FAQs

Breast Reconstruction: Common Questions
- What are some of the advantages to breast reconstruction?
In addition to feeling more “balanced” in weight and appearance after reconstruction, studies show that, women who undergo breast reconstruction have a significant increase in well-being, vitality, general mental health, and healthy body image compared to women who undergo mastectomy without reconstruction.
- Am I a candidate for breast reconstruction?
Almost all women who will undergo mastectomy, or have undergone one, are candidates for breast reconstruction. Some women with certain medical problems like severe heart disease may not, however, be candidates.
- What is a flap?
When living tissue, along with the blood vessels that supply it, is surgically moved from one part of the body to another, the relocated tissue is called a “flap.”
- What is a perforator flap?
Tissue can be surgically relocated from one part of the body to another to reconstruct a breast. When the tissue being relocated includes just the skin and fatty tissue needed for the reconstruction (but does not include any muscle), it is referred to as a perforator flap. Perforator flaps represent a crucial improvement in natural-tissue breast reconstruction because functional muscles are preserved with these procedures. This means that the place where the tissue is taken from heals more quickly, with less pain than with other methods of reconstruction, and without muscle destruction and resultant weakness.
- How do I know if I am a candidate for a perforator flap breast reconstruction?
It is extremely rare for a woman not to have some appropriate place on her body from which tissue can be taken for a perforator flap breast reconstruction.
Because there are so many potential donor site options (including the abdomen, buttocks, thigh, “love-handles” and back), it is almost always possible for an experienced microsurgeon to be able to reconstruct a breast using a perforator flap. Almost all women have enough tissue that can be borrowed from one location or another to reconstruct a breast that will be in proportion to body size. This includes women who have had radiation therapy, women who will require chemotherapy after surgery, thin women, overweight women, women with cancer, women who have had a tummy tuck or other abdominal surgery and, not infrequently, even women who have been told by other health care providers that they are not candidates for breast reconstruction.
- Where does the skin and other tissue come from for natural tissue breast reconstruction?
Procedures that use a woman’s own natural tissue to restore a breast are referred to as autologous or autogenous breast reconstructions. Tissue can be borrowed from a number of different places on the body, including the abdomen, buttocks, love-handle area, thighs and back. Personal preference and body shape will determine the best donor site. Because the tissue comes from your own body, it cannot be rejected.
- When can I have breast reconstruction surgery – can it be done at the same time as my mastectomy?
Breast reconstruction surgery can be performed at the same time as a mastectomy, or it can be performed at a later date. In some cases, the choice between immediate and delayed breast reconstruction is entirely a patient’s own. In other cases, your breast surgeon or oncologist may make specific recommendations about the timing of restorative breast surgery. If you are a candidate for immediate reconstruction (that is, reconstruction of your breast in the same operation as the mastectomy surgery), this option usually offers the best possible cosmetic results. If the recommendation of your doctor is that you wait for some weeks or months, know that successful breast reconstruction can take place after your initial surgery.
- How long after chemotherapy or radiation therapy can breast reconstruction be done?
Successful breast reconstruction can take place months or even years after mastectomy. When chemotherapy is given prior to mastectomy (neo-adjuvant chemotherapy), a period of four to six weeks is typically required before surgery in order to allow a woman’s body to recuperate sufficiently. Even if a person requires chemotherapy after surgery (adjuvant chemotherapy), breast reconstruction can typically still be done at the same time as the mastectomy. When radiation therapy is part of a comprehensive breast cancer treatment plan, we prefer to wait to perform the breast reconstruction until approximately six months after the completion of radiation. Delaying gives the skin time to heal from the effects of radiation, reduces postoperative complications and improves aesthetic outcomes.
- Will I have sensation in my reconstructed breast?
While natural tissue reconstruction does not restore totally normal sensation to your breast, it is sometimes possible to microsurgically connect a sensory nerve in a perforator flap to a sensory nerve at the mastectomy site and restore some degree of sensation to a reconstructed breast. Even when a sensory nerve is not directly connected, small nerve endings (that are cut when a mastectomy is performed) not infrequently grow into the tissue of a natural tissue breast reconstruction and provide some degree of sensation. Since nerves cannot grow into a breast prosthesis, implant reconstructions do not regain sensation.
- What are the benefits of using my own body’s tissue for breast reconstruction as compared with having a breast reconstructed with an implant?
Perhaps the most significant benefit to natural-tissue breast reconstruction is the ability to restore a breast that not only looks and feels much like a normal breast, but which is also a woman’s for the rest of her life. Since the tissue is your own, it cannot be rejected and it is not subject to “wear and tear” like a breast implant. In addition, the tissue of the reconstructed breast will fluctuate in size if your body’s weight changes, helping to maintain the breast’s proportion to the rest of your body. As a woman ages, a natural-tissue breast reconstruction will undergo age- appropriate changes, helping to maintain a natural look.
Implants, on the other hand, are subject to wear and tear, and the outer envelope of an implant can breakdown over time. According to one of the world’s largest manufacturers of breast implants, “breast implants are not considered lifetime devices. You will likely undergo implant removal with or without replacement over the course of your life.” A capsular contracture, one of the most common complications of breast implant reconstruction, can cause aesthetic deformity or pain, and as a result, it is one of the most frequent causes of unanticipated re-operation in women who undergo breast reconstruction with implants. Additional surgery is often needed to address other implant related problems such as: leakage, deflation, erosion through the skin or shifting of the implant into an undesirable position.
>>Read more about breast reconstruction without implants on Medicinenet.com
- Are there advantages to implant breast reconstruction?
Implant surgery requires less extensive surgery than other reconstruction methods, and it usually requires a shorter hospital stay and shorter initial recovery time compared with most other reconstruction options. Implant reconstruction may also be an option for women who are not healthy enough to undergo more complex methods of reconstruction. Because there is no need to collect tissue from another site on the body, reconstruction with implants usually results in only one or two scars on the breast (there is no scarring elsewhere on the body). On the other hand, most women appreciate the tummy-tuck effect that is achieved with a DIEP flap or SIEA flap or the buttock lift effect that is achieved with a LAP flap breast reconstruction as well as the long-term durability of natural-tissue reconstruction.
- What is microsurgery, and why is it used in breast reconstruction?
Microsurgery involves the use of a specialized operating room microscope and instruments to allow a specially trained surgeon to connect extremely small blood vessels and nerves. Microsurgery has revolutionized breast reconstruction surgery because a skilled microsurgeon performing perforator flaps can transfer the skin and fat needed to reconstruct a breast without moving any muscle tissue. Importantly, a breast reconstructed with a perforator flap will be formed with tissue which is alive—not with synthetic or other artificial substances— it is woman’s forever.
- What is a DIEP flap?
DIEP is an acronym for Deep Inferior Epigastric Perforator. The deep inferior epigastric artery and vein, by way of their branches––called perforators––provide the major source of blood supply to the skin and soft tissue of the abdomen. This tissue can be transferred to the chest for use as a DIEP flap breast reconstruction without removing any muscle from the abdomen. Unlike the traditional TRAM flap, the DIEP procedure spares the rectus abdominis muscle because it is based on small vessels that are microscopically separated from the muscle, leaving the muscle intact.The tissue removed from the abdomen for a DIEP flap breast reconstruction is similar to that removed during a tummy-tuck and, as a result, the contour of the abdomen is often improved after breast reconstruction by this method. Because the DIEP flap procedure does not sacrifice muscle, postoperative pain is minimized and abdominal strength is preserved.
- What is an SIEA flap?
SIEA is an acronym for the Superficial Inferior Epigastric Artery. Flaps that utilize this blood vessel for nourishment are termed SIEA flaps. Because this blood vessel travels just below the surface of the skin of the abdomen, no muscle is even touched during surgery when SIEA flaps are used in breast reconstruction. In most women, this vessel is extremely tiny, so it is not a first choice for most breast reconstruction procedures, however, in about 5% to 10% of women, it is large enough to make this procedure a good option. The skin and fat that are removed from the abdomen for an SIEA flap are the same as would be removed for a DIEP flap, and the final decision as to which of these procedures will be performed is made during surgery. As is the case with the DIEP flap, the contour of the abdomen is often improved after breast reconstruction with this flap, the rectus abdominis muscle remains intact, postoperative pain is minimized and abdominal strength is preserved.
- How do DIEP flaps and SEA flaps differ from TRAM flaps?
A Tansverse Rectus Abdominus Myocutaneous (TRAM) flap uses the skin, fat, and underlying rectus muscle to reconstruct a woman’s breast. Women who undergo a TRAM flap frequently experience abdominal weakness from muscle loss. They also incur a significant risk of developing abdominal hernias or bulging of the lower abdomen after surgery. Synthetic mesh is commonly used to reinforce the abdominal wall of patients who have TRAM flap procedures—mesh is not needed in patients who have perforator flap procedures. Because muscle is divided and removed from the abdomen with a TRAM flap, recovery time is generally longer than with other methods of breast reconstruction. When both breasts are reconstructed with TRAM flaps, both rectus abdominis muscles are removed and the incidence of postoperative weakness, hernias and bulges increases further.
The DIEP, SIEA and TRAM flaps all use almost exactly the same skin and fatty tissue, importantly, however, the “six-pack” rectus abdominus muscle is preserved with the DIEP and SIEA flaps. Because DIEP and SIEA flaps preserve these large abdominal wall muscles, recovery is typically quicker and less painful than recovery from a TRAM flap.
- What is a GAP flap?
GAP is an acronym for Gluteal Artery Perforator. The gluteal artery, via its branches called perforators, supplies the skin and fat of the buttock area. When tissue is collected and transferred using the gluteal artery to provide blood supply, it is called a GAP flap. When the upper buttock is used, the reconstruction is referred to as an SGAP, and when the lower buttock is used, an IGAP. GAP flaps are an excellent option for women who do not have enough tissue on their abdomen or who cannot or do not want to use their abdomen to reconstruct breasts of their desired size.
How does the “Stacked DIEP Flap” allow women to use their abdomen for breast reconstruction when there is “not enough tissue” for other abdominal flaps?
The Stacked-DIEP flap procedure uses two DIEP flaps (one DIEP flap from each side of the abdomen) to reconstruct a single breast. These procedures allows a breast to be reconstructed with significantly more tissue than can be obtained with either a single DIEP flap or a TRAM flap.
- If I do not want to, or cannot use my abdomen or buttocks for a perforator flap breast reconstruction, are there other perforator flap options?
In addition to the abdomen and the buttocks, the inner thigh, the “love handle” areas, hips and lower back, as well as the upper back are all possible donor site options. The Lumbar Artery Perforator (LAP), Transverse Upper Thigh (TUT or TUG) and Thoracodorsal Artery Perforator (TAP or TDAP) flaps are excellent alternative flaps.
- Why is it that so few surgeons perform perforator flaps such as the DIEP, SIEA and GAP flaps?
Perforator flap microsurgery is complex and time consuming. Many plastic surgeons do not have the training or experience needed to perform these technically challenging procedures with a high degree of success. Furthermore, efficiency and success are improved by a team approach and commitment to performing these procedures on a regular basis and following patients ourselves very closely after surgery. Dr. Greenspun always performs perforator flap surgery with another microsurgeon specifically trained in perforator flap breast reconstruction techniques. There are only a few such highly skilled breast reconstruction teams.
- How long does perforator flap surgery take tor perform?
Typically, reconstruction of one breast takes between four and five hours, while reconstruction of both breasts takes between six and a half and eight and a half hours to perform. Even tough this may seem like a long time to be in surgery, patients generally recover very quickly. Most patients are able to get out of bed after breakfast on the first morning after surgery.
- How long will it take for me to get back to my normal routines and exercise after a perforator flap breast reconstruction?
Although the length of recovery varies somewhat with each procedure, and is different for each individual, most patients will spend four nights in the hospital so to be monitored effectively by the surgical team. While in the hospital, patients recuperate in a private room. If you follow post-operative instructions carefully, you will be able to enjoy your normal activities within a relative short period of time.
Here is what to expect when recovering from a perforator flap breast reconstruction:
As you recover at home during the first weeks after surgery, you will be asked to avoid vigorous or strenuous activity. Many women are able to drive within two weeks of perforator flap surgery. Women can typically return to non-manual labor such as office work within two to three weeks. Most people can resume light exercise by four weeks and can resume more vigorous physical activity by six to eight weeks. Because there is variation from person to person, it is very important to check with us before resuming any physically demanding work or beginning an exercise regimen.
Recovery following the second stage of reconstruction (outpatient procedure that can include nipple reconstruction and refinement of breast shape) is usually much quicker and less restricted; you will likely be able to return to your normal routine after just a few days and to vigorous exercise within two weeks.
- What if my breast cancer comes back after I have had a breast reconstruction?
Studies published in peer-reviewed journals have shown that breast reconstruction does not make breast cancer more likely to re-occur. Furthermore, reconstruction has not been shown to negatively impact on a women’s chance of cure in the event a recurrence occurs. In cases where cancer recurs after reconstruction, further treatment (surgery, chemotherapy, radiation) is undertaken as necessary. Often, treatment can be done without removing the reconstructed breast if a woman’s breast was restored using her own tissue.
- Will my health insurance plan cover the cost of breast reconstruction with a DIEP, SIEA, GAP or other perforator flap?
Federal and state laws protect a woman’s right to have her breasts reconstructed after mastectomy. In 1998, the Federal Breast Reconstruction Law was passed requiring insurance providers to cover breast reconstruction surgery and any surgery operations to create symmetry in either breast if they provide coverage for mastectomy. If your insurance provides coverage for a mastectomy, it must provide coverage for the method of reconstruction you choose. Breast reconstruction is not subject to review for medical necessity. If a surgeon in your network of participating providers does not offer the method of reconstruction you are seeking, your insurer must still provide coverage. If necessary, your insurer may have to provide coverage for you to have reconstruction performed by a non-participating physician even if that means you will need to travel to another city or state.
For women who do not have access to a network-participating physician who performs these procedures, we are often able to obtain exceptions for treatment outside of the participating-provider network. If you want to have a perforator flap breast reconstruction, but your insurance carrier cannot find a network-participating provider offing you this kind of breast reconstruction, our office staff can help you to try to obtain the necessary authorization for treatment outside of your network. In all cases, we will work closely with you and your insurance carrier to minimize your out-of-pocket expenses for surgery.
Breast Reconstruction in New York and Connecticut
Our practice specializes in the most advanced methods of natural-tissue breast restoration. Certified by the American Board of Plastic Surgery, Dr. Greenspun specializes in microsurgical breast reconstruction surgery including DIEP, SIEA, SGAP, IGAP, LAP and TUG flap surgery. Our offices are located in New York City and Greenwich, Connecticut.
Presurgical Planning

Pre-Operative Blood Vessel Mapping
There is significant variability from one person to another, in the anatomy of the small blood vessels known as “perforators,” and this contributes to the complexity of perforator flap breast reconstruction surgery. Dr. Greenspun is recognized as an expert in the field of preoperative perforator flap blood vessel imaging. He has lectured at meetings around the world about the non-invasive imaging techniques that he helped to develop to improve perforator flap surgical flap outcomes. The ability to establish a “map” of each patient’s blood vessels before surgery dramatically reduces the time it takes to perform these procedures and, importantly, allows surgery to be performed with the highest possible degree of safety and efficacy. Without pre-operative blood vessel imaging, a surgeon will not be able to see a patient’s vessels until surgery is underway.
Together with radiologists at Montefiore Medical Center, Dr. Greenspun has developed specialized techniques that use magnetic resonance imaging (MRI) to reveal—in medical terms, image—the tiny blood vessels of the abdominal wall before DIEP flap or SIEA flap surgery. Working with radiologists at the Weill Medical College-Cornell University in New York City, he helped develop protocols that allow surgeons to use MRI to map the blood vessels used in various flaps including DIEP flaps, SIEA flaps, SGAP flaps, IGAP flaps, LAP flaps and TUG flaps. Unlike CT-scans, which can also be used to image perforator flap blood vessels before surgery, MRI scans do not expose women to radiation and its potentially harmful effects. Dr. Greenspun and other perforator flap surgeons now routinely use these imaging techniques to help identify the very best blood vessels for each patient’s reconstruction.
Links

Links
Links to websites that may be valuable to people seeking information about breast reconstruction and breast cancer are proved below. While we think these websites may be helpful, we do not sponsor or endorse these Web sites or the products and services they provide, nor can we guarantee the accuracy of the information contained on them.
BREAST CANCER INFORMATION
- Breastcancer.org
- Breastcancer.org is a nonprofit organization dedicated to providing the most reliable, complete, and up-to-date information about breast cancer.
- American Cancer Society
- The American Cancer Society is a nationwide, community-based voluntary health organization dedicated to eliminating cancer as a major health problem.
- Medline Plus
- MedlinePlus is the National Institutes of Health’s Web site for patients, their families and their friends. Produced by the National Library of Medicine, this resource brings you up-to-date health information in language you can understand.
- National Cancer Institute
- This NCI, part of the National Institutes of Health, is the Federal Government’s principal agency for cancer research and training. The NCI has legislative mandates that include information dissemination to medical professionals and the general public as well as a requirement to assess the incorporation of state-of-the-art cancer treatments into clinical practice
- National Institutes of Health
- The National Institutes of Health (NIH), a part of the U.S. Department of Health and Human Services, is the nation’s medical research agency—making important medical discoveries that improve health and save lives.
- Centers for Disease Control and Prevention
- The CDC′s Mission is to collaborate to create the expertise, information, and tools that people and communities need to protect their health – through health promotion, prevention of disease, injury and disability, and preparedness for new health threats.
- National Breast Cancer Foundation
- The National Breast Cancer Foundation’s mission is to save lives by increasing awareness of breast cancer through education and by providing mammograms for those in need.
- Dictionary of Cancer Terms
- The National Cancer Institute’s Dictionary of Cancer Terms, a resource with more than 6,000 terms related to cancer and medicine.
BRCA & GENETICS
- BRACAnalysis® and Genetic Testing
- BRACAnalysis® is a genetic test to find out if you have a BRCA1 or BRCA2 mutation that increases your risk of developing breast and/or ovarian cancer. More information about this test is available on the Myriad Genetics website
- Breast Cancer Risk Assessment Tool
- The Breast Cancer Risk Assessment Tool is an interactive tool for health designed to be used by healthcare professionals to estimate a woman’s risk of developing breast cancer.
- Facing Our Risk of Cancer Empowered
- The mission of FORCE, the only national nonprofit organization devoted to hereditary breast and ovarian cancer, includes support, education, advocacy, awareness, and research specific to hereditary breast and ovarian cancer.
SUPPORT SERVICES
- Komen Foundation
- As the world’s largest grassroots network of breast cancer survivors and activists, Susan G. Komen for the Cure® is working to save lives, empower people, ensure quality care for all and energize science to find the cures.
- Young Survival Coalition
- Young Survival Coalition is the premier international organization dedicated to the critical issues unique to young women and breast cancer.
- I’m Too Young For This!
- Founded by and for young adults affected by cancer, i2y– The I’m Too Young For This! Cancer Foundation–is the nation’s largest support community for the next generation of patients, survivors and caregivers between 15-40.
- Cancer101
- Cancer101’s mission is to empower cancer patients and their caregivers to take control over their diagnoses from the moment they learn they have cancer, a recurrence or metastases through ten years of follow-up care.
- Living Beyond Breast Cancer
- LBBC is a national education and support organization, whose goal it is to improve your quality of life and help you take an active role in your ongoing recovery or management of breast cancer, regardless of educational background, social support or financial means.
- Gilda’s Club
- The mission of Gilda’s Club is to create welcoming communities of free support for everyone living with cancer – men, women, teens and children – along with their families and friends.
- Network of strength (formerly Y-ME)
- Network of Strength, offers support through information, empowerment and peer support, so that no one has to face breast cancer alone.
- Self-Help for Women with Breast or Ovarian Cancer
- SHARE’s mission is to create and sustain a supportive network and community of women affected by breast or ovarian cancer. SHARE brings these women and their families and friends together with others who have experienced breast or ovarian cancer, and provides participants with the opportunity to receive and exchange information, support, strength and hope.
- Cancercare
- CancerCare is a national nonprofit organization that provides free, professional support services to anyone affected by cancer: people with cancer, caregivers, children, loved ones, and the bereaved. CancerCare programs—including counseling and support groups, education, financial assistance and practical help—are provided by professional oncology social workers and are completely free of charge.
PLASTIC SURGERY
- The Breast Reconstruction Guide Book
- The second edition of The Breast Reconstruction Guidebook will help you understand what to expect from mastectomy, sort through the benefits and limitations of reconstructive procedures, and decide which, if any, reconstruction is right for you.
- DIEP Sisters
- This website was created by and for women who are looking for information on Breast Cancer and Breast Reconstruction from people who have been through it.
- DIEPBreastReconstruction.org
- A breast reconstruction patient’s thoughts about DIEP flap breast reconstruction presented with helpful information about choosing a surgeon, if perforator flap breast reconstruction is appealing to you
- American Society of Plastic Surgeons
- The American Society of Plastic Surgeons (ASPS) is the largest plastic surgery specialty organization in the world. Founded in 1931, the society is composed of board-certified plastic surgeons. The mission of the society is to advance quality care to plastic surgery patients by encouraging high standards of training, ethics, physician practice and research in plastic surgery.
BREAST IMPLANTS
- Food And Drug Administration – Guide to Breast Implants
- FDA’s mission is to assure that the products that it approves are safe and effective. Information on the FDA’s website is intended to help you make an informed decision if you are considering breast implants.
- Food And Drug Administration – Implant Consumer Information
- FDA’s mission is to assure that the products that it approves are safe and effective. Information on the FDA’s website is intended to help you make an informed decision if you are considering breast implants.
- Institute of Medicine – Report on the Safety of Silicone Implants
- The IOM is the health arm of the National Academy of Sciences, an honorific society of distinguished scholars that serves as advisors to the government on issues of the nation’s health. The IOM’s Committee on the Safety of Silicone Breast Implants issued a detailed report on the safety of breast implants.
CLINICAL TRIALS
- Clinical Trials
- ClinicalTrials.gov is a registry of federally and privately supported clinical trials conducted in the United States and around the world. ClinicalTrials.gov gives you information about a trial’s purpose, who may participate, locations, and phone numbers for more details.
- Center Watch – Clinical Trials Information
- CenterWatch is a trusted source and global destination for clinical trials information for both professionals and patients. CenterWatch is committed to providing patients and their advocates information on clinical trials, specific drugs, as well as other essential health and educational resources.
- American Cancer Society- Guide to Clinical Trials
- The American Cancer Society Clinical Trials matching Service is a free, confidential program that helps patients, their families and health care workers find cancer clinical trials most appropriate to a patient’s medical and personal situation.
- National Institutes of Health- Clinical Trials
- Find information about clinical trials at the National Cancer Institute’s website. Learn about clinical trials, browse results of recent clinical trials and find trials accepting new patients.
Our Practice Portal

Breast Reconstruction in Connecticut and New York
New Patient Forms
For our practice to deliver the best possible care to all our patients, we need to know as much about your medical history as possible. Please download, print and fill out these patient information forms prior to your first office visit. Be sure to bring a copy of your completed forms with you to this appointment along with your insurance card and copies of any current mammogram or pathology reports that you may have. Should you have any questions or require assistance, please call our office.
New Patient Registration Form (PDF)
Preparing for Perforator Flap Surgery
Our “Perforator Flap Breast Reconstruction Information Booklet” contains valuable information that will help you to prepare for surgery and your recovery.
Perforator Flap Breast Reconstruction Information Booklet (PDF)
Preoperative Medical Clearance
You will be asked to see your primary care doctor/internist for a general medical evaluation, usually within the month prior to surgery. Your will need to present your primary care doctor with a letter that describes your planned procedure, so that he or she will be sure to understand the nature of your upcoming surgery. Select the request for medical clearance letter that describes your planned procedure and print out a copy to take to your doctor.
Recovering After Perforator Flap Breast Reconstruction Surgery
After your return home from the hospital, please know that our practice wants to help you recover as smoothly as possible, so feel free to call our office with any questions or concerns. Much of what you can expect during your recovery is outlined in our “Perforator Flap Breast Reconstruction Information Booklet.”
Postoperative Instructions (PDF)
During your recovery, if you notice any of the following, please notify Dr. Greenspun immediately:
- A change in color of the skin of your reconstructed breast/s
- Severe pain not alleviated by pain medication
- Sudden swelling at a surgical site
- Severe swelling at a surgical site
- A sudden increase in the amount of fluid in the drain reservoirs, or more than 100cc of drain output in a 24-hour period
- Redness, warmth, or hardening of a surgical site
- Bleeding
- Odorous drainage or pus
- A temperature of 100 degrees or more that lasts over 8 hours or a temperature higher than 101.5
- Any worrisome symptom
Recovering After Stage II Breast Reconstruction Surgery
About three months after the first stage of reconstruction, many women elect to have a relatively short outpatient procedure to reconstruct nipples and refine the shape of their reconstructed breasts. Most women recover from this procedure rapidly and require little if any time away from work.
Postoperative Instructions for Stage II Surgery (PDF)
Nipple and Areola Tattoo
At an outpatient visit about 6 to 8 weeks after Stage II, the reconstructed nipple and the area around it can be tattooed to fully restore the appearance of a normal nipple and areola.
Post-Procedure Instructions and Tattoo Care (PDF)
Patient Letters
We hope that sharing some of our patients’ observations will help you better envision the compassionate and personalized patient-centered care our practice provides, and also offer some direct insight into our patients’ experiences.
Breast Implant Associated-Anaplastic Large Cell Lymphoma

Breast Implant Associated-Anaplastic Large Cell Lymphoma
Recent warnings from the Food and Drug Administration (FDA) linking some breast implants with a type of non-Hodgkin lymphoma have generated concern for women with breast implants and for the medical community. There is no cause for panic at this time, but it is important that all women who have, or have had breast implants, or are considering breast implants, inform themselves about the association of breast implants with Anaplastic Large Cell Lymphoma (ALCL).
In late January 2011, the FDA raised concerns about a link between breast implants and a rare form of lymphoma, called ALCL, a cancer of the cells of the immune system. Since FDA publicized the initial reports, many additional cases of breast implant associated ALCL or BIA-ALCL have been reported. Current data suggest that the risk of BIA-ALCL is highest for women who have, or who have had “textured” surface breast implants.
At the present time, reports in the medical literature estimate that BIA-ALCL may occur in roughly 1 in 3,000 to 1 in 30,000 women with textured breast implants. In comparison, without breast implants, the incidence of ALCL of the breast is only about 3 in 100,000,000 according to the FDA.
As of late 2018, the FDA advises the following:
- Women should continue monitoring their implants and obtaining regular breast screening evaluations.
- Women who see changes in the way the area around a breast implant looks or feels—including swelling, lumps or pain around the implant—should promptly see a physician for evaluation.
- If a woman with breast implants has no symptoms, at this time, FDA is not recommending the routine removal of breast implants.
- Continue routine MRI evaluation for “silent rupture” if you have silicone-filled implants.
Based upon the best currently available data, we believe that women opting for breast implants either for cosmetic or reconstructive purposes, should strongly consider using only smooth-surface tissue expanders and implants. The surgeons of the Advanced Reconstructive Surgery Group feel so strongly about this, that we have abandoned the use of textured tissue expanders and textured breast implants in our practice.
Women considering breast implants should inform themselves about BIA-ALCL and weigh the risks, the uncertainty, and the potential benefits of breast implants for themselves.

