Perforator Flap Procedures
Natural Tissue Breast Reconstruction with Perforator Flaps
Perforator flaps represent the current state-of-the-art in natural tissue breast reconstruction. Depending on the shape of your body and your personal preference, several areas of the body can act as donor sites for the tissue needed to restore the shape and form of the breast.
Perforator flap options for breast reconstruction include:
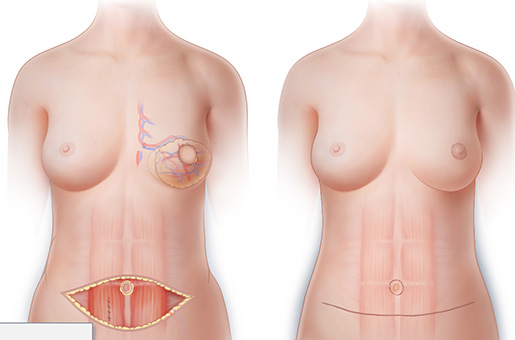
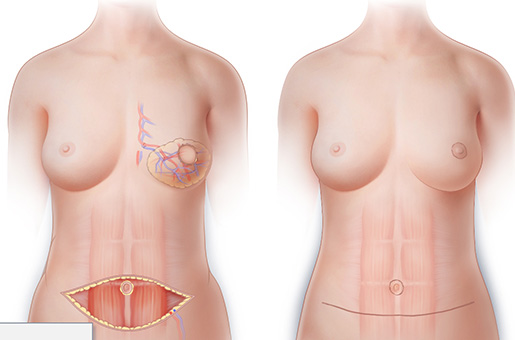
Using an incision similar to that used for a “tummy tuck,” skilled surgeons can reconstruct a breast from skin and fatty tissue taken from the lower abdomen—without removing any muscle.
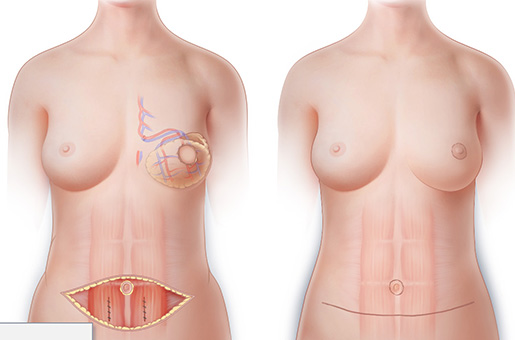
This innovative procedure uses two DIEP flaps, one DIEP flap from each side of the abdomen, to reconstruct a single breast. The Stacked-DIEP flap allows a single breast to be reconstructed with significantly more tissue than is possible using either a DIEP flap or a TRAM flap.
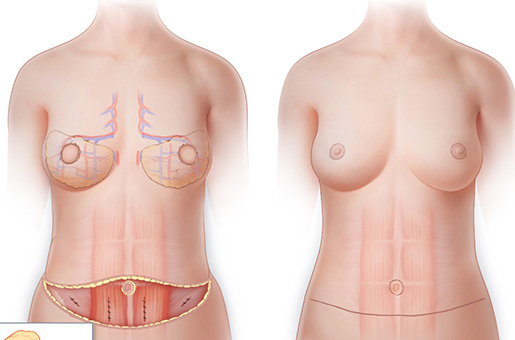
BODY LIFT BREAST RECONSTRUCTION WITH EXTENDED DIEP FLAPS
When there is not enough lower abdominal tissue to reconstruct both breasts to the desired size, the tissue of the flanks, hips or upper buttocks can be combined with tissue of the lower abdomen to achieve results not possible with ordinary perforator flaps.
Similar to DIEP flaps, in that they use skin and fat from the lower abdominal area for breast reconstruction, SIEA flaps allow for breast reconstruction using lower abdominal tissue without muscle destruction.
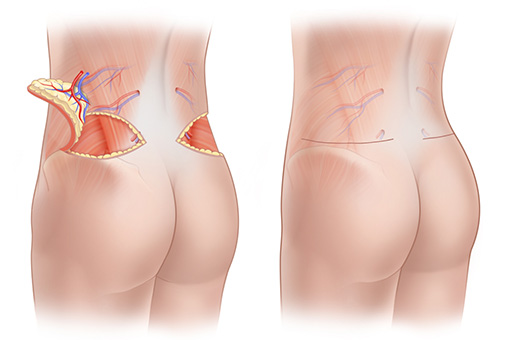
Using tissue fatty tissue from the “love-handle” area, is possible to reconstruct a woman’s breasts and at the same time, sculpt the lower back and lift the buttock.
THE THIGH AS A DONOR SITE: PAP, DUG AND TUG FLAPS
The skin and fat of the upper thigh can also be used to reconstruct breasts with a natural appearance. Depending on the shape of the thigh and the distribution of fatty tissue, a PAP flap, DUG flap or TUG flap may be most appropriate.
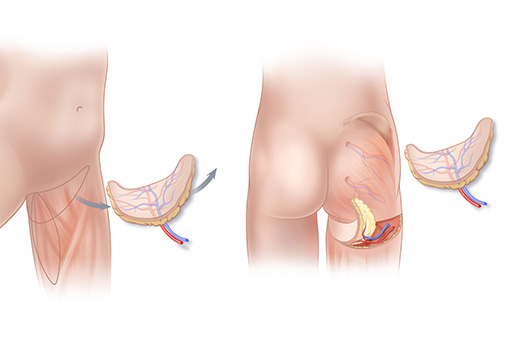
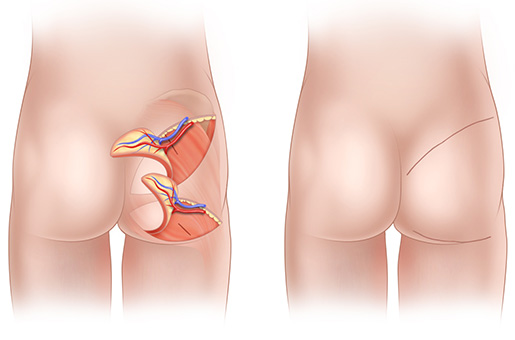
For women who cannot use—or choose not to use—tissue from their abdomen, lumbar area, or thighs, SGAP and IGAP flaps are an alternative for natural-tissue breast reconstruction after mastectomy. Without removing any muscle tissue can be borrowed from the upper (SGAP) or lower (IGAP) buttock.
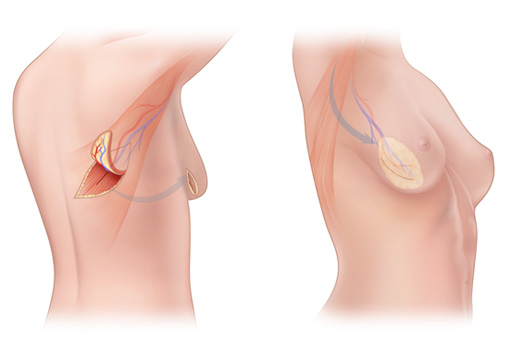
The Thoracodorsal Artery Perforator flap, known as a TDAP or TAP flap, is a perforator flap that can be rotated from the upper back to the chest for use in breast reconstruction.